Key points
- Up to 225 cases of Hansen's disease are identified in the U.S. every year.
- There are three types of Hansen's disease, each with slightly different signs and symptoms.
- In the U.S., people with the disease may be treated at specialized clinics run by the National Hansen's Disease Program. There are several federally supported outpatient clinics throughout the country.
- Hansen's disease can be cured with multidrug therapy, which consists of a combination of antibiotics.

Etiology
Hansen's disease is caused by an acid-fast rod-shaped bacillus Mycobacterium leprae and Mycobacterium lepromatosis. The organism multiplies very slowly (dividing approximately once every 13 days).
It is an obligate intracellular pathogen that lacks several genes needed for independent survival. Thus, it has never been grown in bacteriologic media. However, it has been grown in mouse foot pads.
At-risk populations
Hansen’s disease is very rare in the United States, with around 150 cases reported per year. Most people with Hansen’s disease in the U.S. became infected in a country where it is more common.
However, there have been cases of Hansen's disease reported in U.S. residents with no international travel.
Signs and symptoms
There are three types of Hansen's disease, each with slightly different signs and symptoms. Sometimes, there are other clinical presentations due to the diseases wide range of possible clinical manifestations.
This is the most common form of Hansen's disease. Skin lesions are numerous and may be found anywhere on the body. Peripheral nerves are affected as well, with ensuing weakness and loss of sensation.
PB Hansen's disease is characterized by hypopigmented or hyperpigmented skin macules that exhibit loss of sensation. This is due to infection of the peripheral nerves supplying the region. The body's immune response may also result in swelling of the peripheral nerves. These enlarged nerves may be palpated under the skin and may be tender to the touch.
The nerves most likely to swell are:
- Great auricular nerve
- Ulnar nerve above the elbow and dorsal cutaneous branches at the wrist
- Median nerve at the wrist (in the carpal tunnel)
- Radial nerve (superficial at wrist)
- Common peroneal nerve
- Posterior tibial nerve, posterior to the medial malleolus
- Sural nerve




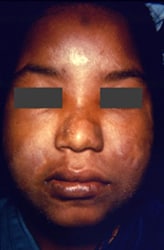
MB Hansen's disease is characterized by generalized or diffuse involvement of the skin and a thickening of the peripheral nerves. It has the potential to involve other organs, the eyes, nose, testes, and bone. The nodular form of this condition is the most advanced form of the disease. Ulcerated nodules contain large numbers of M. leprae acid-fast bacilli packed in macrophages that appear as large foamy cells.
MB Hansen's disease is associated with:
- Multiple, symmetrically distributed skin lesions
- Nodules
- Plaques
- Thickened dermis
- Involvement of the nasal mucosa resulting in congestion and epistaxis

Corneal ulcer
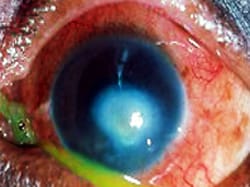
Staphyloma

Nose skin changes

Ear lesion

Treatment and recovery
Hansen's disease is treated with multidrug therapy using a combination of antibiotics depending on the form of the disease:
- PB Hansen's disease:
- Daily dapsone and rifampicin once per month
- Daily dapsone and rifampicin once per month
- MB Hansen's disease:
- Daily clofazimine is added to rifampicin and dapsone.
- Daily clofazimine is added to rifampicin and dapsone.
Once treatment begins, the patient is no longer considered infectious. Treatment usually lasts one to two years. Hansen's disease can be cured if treatment is completed as prescribed.
Spotlight
World Health Organization (WHO) published a detailed guide to classification and treatment of leprosy.
At least one in four patients with Hansen's disease experience reactions during treatment. Reactions may occur before treatment begins or after it is completed. Reactions are not due to medications used to treat the disease, although people treated with clofazimine tend to have slightly fewer episodes.
There are two main groups of reactions:
- Type 1 reactions, also called reversal reactions, are typical in PB and borderline Hansen's disease. They show up as edema and erythema of pre-existing lesions. In some cases, neuritis and, rarely, new lesions or fever may occur.
- Type 2 reactions, or Erythema nodosum leprosum (ENL), are most frequently seen in patients with MB Hansen's disease. Patients usually present with painful erythematous nodules, often distributed between existing lesions, and moderate to high fever. Inflammation of other tissues may be present, including peripheral neuritis, orchitis, lymphadenitis, iridocyclitis, nephritis, periostitis and arthralgias.
Lucio's phenomenon is a rare reaction of hard-to-heal ulcers, typically seen in patients of Mexican ancestry with MB Hansen's disease.

Long-term effects
Over time, if Hansen's disease is not treated, the following complications can occur:



