Key points
- Each year, up to 225 people in the U.S. and 250,000 around the world are diagnosed with Hansen's disease (also known as leprosy).
- Hansen's disease was once feared as a highly contagious, devastating disease.
- Now, we know that it's hard to spread and easily treatable.
- People with Hansen's disease can live an active life during and after treatment.
More Information
What it is
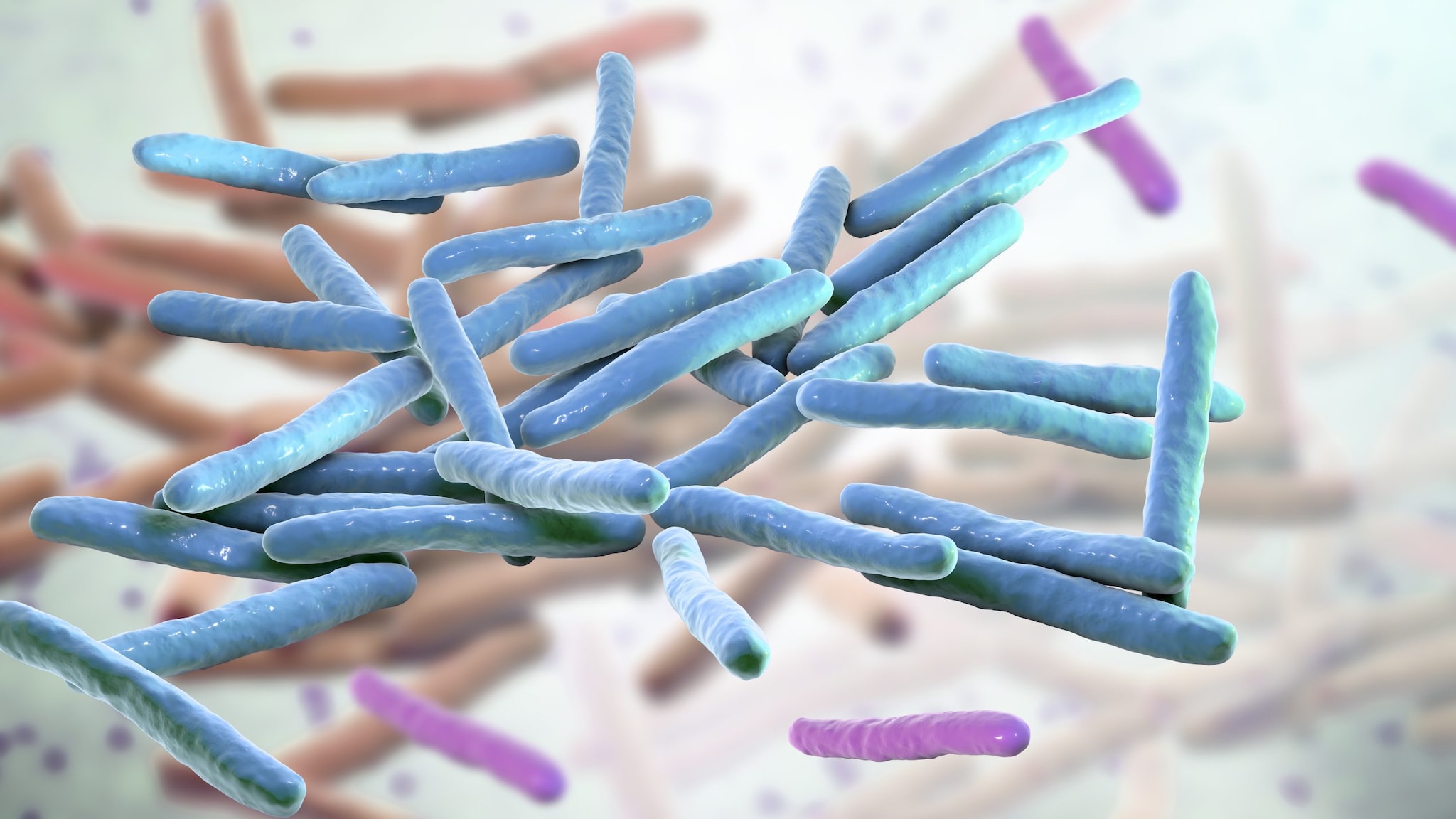
Hansen's disease is caused by slow-growing bacteria called Mycobacterium leprae and Mycobacterium lepromatosis. The disease can affect the nerves, skin, eyes, and lining of the nose. In some cases, body parts may lose their sense of touch and pain, increasing the likelihood of injuries such as cuts and burn.
Despite the disease being hard to catch and completely curable, a lot of stigma and prejudice remains against those who have Hansen's disease. Individuals affected by the disease often face social isolation and discrimination, particularly in regions where the illness is prevalent.
Signs and symptoms
Symptoms mainly affect the skin, nerves, and lining of the nose.
How long it takes for signs to show
The bacteria that causes Hansen's disease grows very slowly. After contact with the bacteria, it may take up to 20 years for someone to develop signs of the disease.
Risk factors
In the United States, Hansen's disease is rare. Most people with Hansen's disease in the U.S. became infected in a country where it is more common.
You may be at risk for the disease if you live in a country where the disease is widespread. According to WHO data from 2019:
- Brazil, India and Indonesia reported more than 10,000 new cases
- Bangladesh, Democratic Republic of the Congo, Ethiopia, Madagascar, Mozambique, Myanmar, Nepal, Nigeria, Philippines, Somalia, South Sudan, Sri Lanka and the United Republic of Tanzania each reported 1000–10,000 new cases.
How it spreads
Most people cannot get Hansen's disease
Testing and diagnosis
Healthcare providers can diagnose Hansen's disease by conducting an exam and running diagnostic tests, like skin biopsies. They may look for patches of skin that may look lighter, darker, or redder than the person's normal skin and determine if those patches have a loss of feeling.
To confirm the diagnosis, healthcare providers will take a skin or nerve sample to look for the bacteria that cause Hansen's disease under the microscope. They may also do tests to rule out other skin diseases.
Treatment and recovery
Hansen's disease is treated with a combination of antibiotics. Treatment usually lasts between one to two years. The illness can be cured if treatment is completed as prescribed.
In the U.S., people with Hansen's disease may be treated at specialized clinics run by the National Hansen's Disease. There are several federally supported outpatient clinics throughout the U.S. and Puerto Rico.
Myths and misconceptions
Myth: Hansen's disease is very contagious.
Fact: Hansen’s disease does not spread easily from person to person. You cannot get it through casual contact such as shaking hands, sitting next to, or talking to someone who has the disease.
Myth: There is no cure for Hansen's disease.
Fact: Hansen's disease is curable. People being treated for Hansen's disease can live a normal life among their family and friends and can continue to attend work or school.
Myth: Hansen's disease makes your fingers and toes fall off.
Fact: Fingers and toes do not just “fall off” due to Hansen's disease. The bacteria that cause the disease attacks the nerves of the fingers and toes, causing them to become numb. Injuries like burns, ulcers, and cuts on numb parts can go unnoticed, which may lead to permanent damage or infection, causing loss of the digit. Sometimes, the nerve damage makes muscles in the fingers and toes so weak that the muscles and bones begin to disintegrate and be reabsorbed by the body.
- Britton WJ, Lockwood NJ. Leprosy. Source: Lancet. 2004;363:1209-1219.
- Bruce S, Schroeder TL, Ellner K, Rubin H, Williams T, Wolf JE Jr. Armadillo exposure and Hansen's disease: an epidemiologic survey in southern Texas. Source: J Am Acad Dermatol. 2000;43(2 Pt1):223-228.
- Hansen's Disease | Technical Instructions for Civil Surgeons | Immigrant and Refugee Health | CDC Last updated: 2024 May 14. Accessed: 2024 June 6.
- Hartzell JD, Zapor M, Peng S, Straight T. Leprosy: a case series and review. Source: South Med J. 2004;97:1252-1256.
- Martiniuk F, Rao SD, Rea TH, et al. Leprosy as Immune Reconstitution Inflammatory Syndrome in HIV-positive Persons. Source: Emerging Infectious Diseases. 2007;13(9):1438-1440. doi:10.3201/eid1309.070301.
- Nolen L, Haberling D, Scollard D, et al. Incidence of Hansen's Disease — United States, 1994–2011. Source: Morbidity and Mortality Weekly Report (MMWR). 2014 / 63(43);969-972.
- Ooi WW, Moschella SL. Update on leprosy in immigrants in the United States: status in the year 2000. Source: Clin Infect Dis. 2001;32:930-937.
- Scollard DM, Adams LB, Gillis TP, Krahenbuhl JL, Truman RW, Williams DL. The continuing challenges of leprosy. Source: Clinical Microbiology Reviews. 2006;19(2):338-381.
- Truman, RW, Singh, P., Sharma, R, Busso, JP, Rougemont, J, Paniz-Mondolfi, A, Kapopoulou, A, Brisse, S, Scollard, DM, Gillis, TP, and Cole, ST. Probable Zoonotic Leprosy in the Southern United States. Source: N Engl J Med. 2011;364:1626-1633.
- Williams D, Hagino T, Sharma R, et al. Primary Multidrug-Resistant Leprosy, United States. Source: Emerging Infectious Diseases. 2013;19(1):179-181. doi:10.3201/eid1901.120864.
- Woodall P, Scollard DM, Rajan L. Hansen Disease among Micronesian and Marshallese Persons Living in the United States. Source: Emerging Infectious Diseases. 2011;17(7):1202-1208. doi:10.3201/eid1707.102036.
- World Health Organization. Surveillance of drug resistance in leprosy: 2010. Source: Wkly Epidemiol Rec. 2011;86:237–240.
- World Health Organization. Global leprosy update, 2015: time for action, accountability and inclusion. Source: Wkly Epidemiol Rec. 2016; 91:405–420.
- Worobec SM. Current approaches and future directions in the treatment of leprosy. Source: Res Rep Trop Med. 2012;3:79–91.
