Key points
- Blastomycosis is a lung infection caused by breathing in fungal spores from Blastomyces.
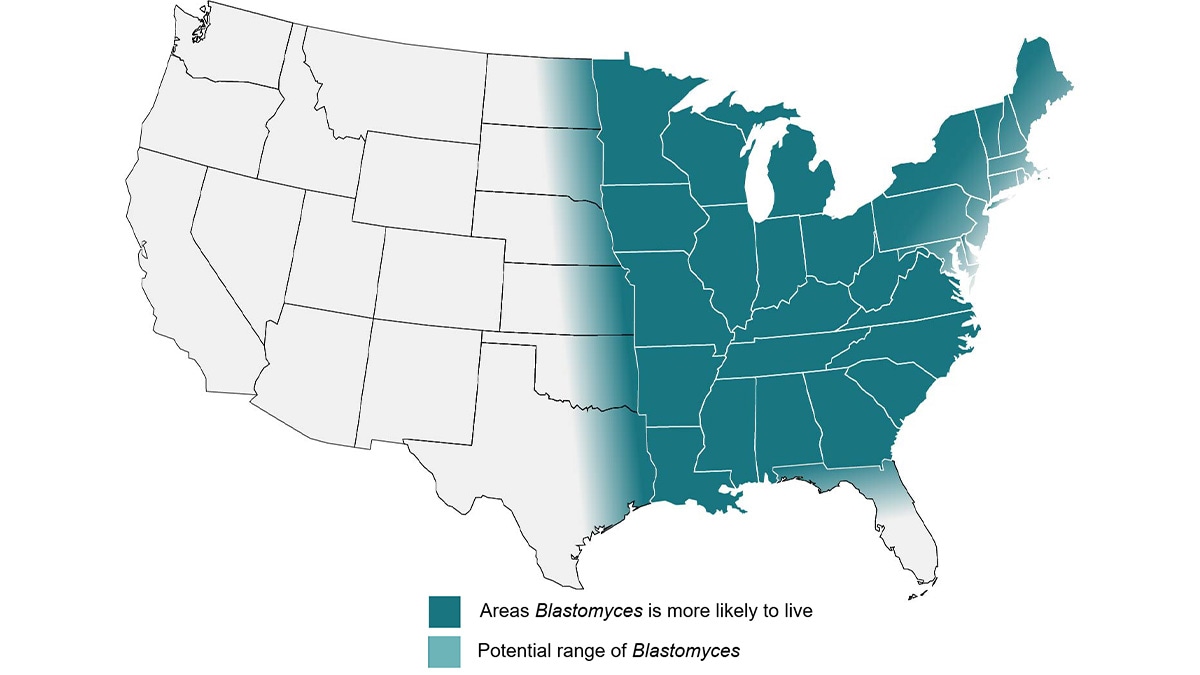
- Blastomyces live in soil in the midwestern, south-central, and southeastern U.S.
- Surveillance research helps estimate areas where Blastomyces live.
- The exact geographic range of the fungus is not known.
- There are no reliable environmental tests for Blastomyces.

Causes
People can get blastomycosis by breathing in Blastomyces, a fungus. The fungus lives in the environment in moist soil and decomposing plant matter like wood and leaves. About half of people who breathe in Blastomyces do not get blastomycosis.
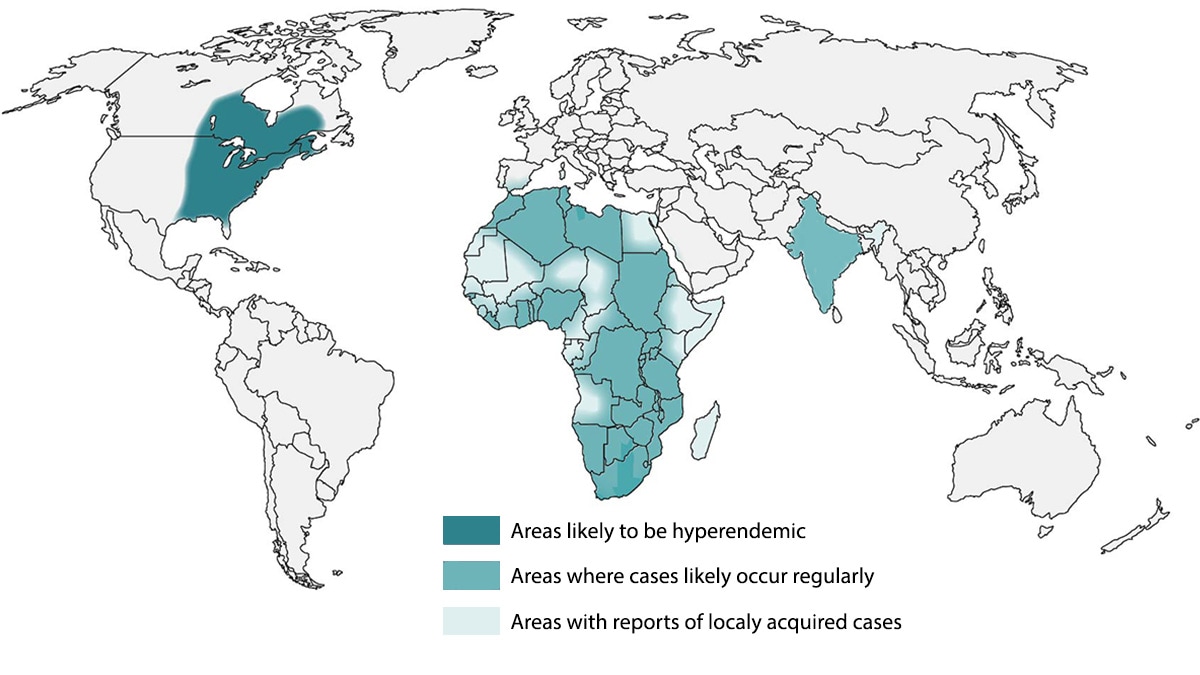
In the United States, the fungus mainly lives in the midwestern, south-central, and southeastern states. It is most common around the Ohio and Mississippi River valleys, Great Lakes, Saint Lawrence River, and western United States. The fungus also lives in Canada and a small number of blastomycosis cases have been reported from Africa and India.
Estimated areas with Blastomyces
These maps show estimates of where the fungus that cause blastomycosis lives.
- Blastomyces is not evenly distributed within the estimated areas.
- The fungus may be present outside of the areas shown.
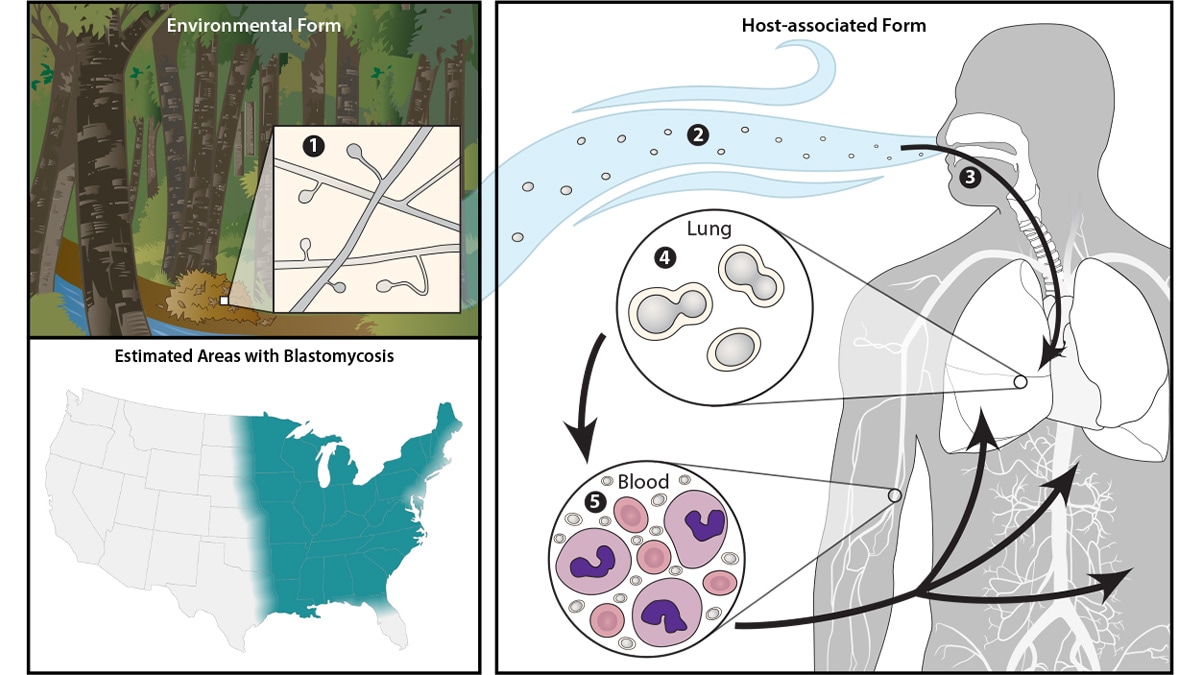
Life cycle of Blastomyces
Blastomyces lives in the environment as a mold that produces fungal spores. The spores are too small to see without a microscope. When soil or plant material is disturbed, the tiny spores can be released into the air. When people or animals breathe in the spores, they are at risk for developing blastomycosis. After the spores enter the lungs, the body temperature allows the spores to transform into yeast. The yeast can stay in the lungs or spread through the bloodstream to other parts of the body, such as the skin, bones and joints, organs, and central nervous system (brain and spinal cord).
Environmental testing
Testing the environment for Blastomyces isn't likely to be useful in most situations. When an environmental sample tests positive for Blastomyces, it isn't necessarily a source of infection, and when a sample tests negative, that doesn't necessarily mean that the fungus isn't there. There are no publicly available tests to detect Blastomyces in the environment. Testing environmental samples for Blastomyces is currently only done for scientific research.
- Furcolow ML, Busey JF, Menges RW, Chick EW. Prevalence and incidence studies of human and canine blastomycosis. II. Yearly incidence studies in three selected states, 1960–1967. Am J Epidemiol. 1970;92(2):121–31.
- Bradsher RW, Chapman SW, Pappas PG. Blastomycosis. Infect Dis Clin North Am. 2003;17(1) 21-40, vii.
- Morris SK, Brophy J, Richardson SE, Summerbell R, Parkin PC, Jamieson F, et al. Blastomycosis in Ontario, 1994-2003. Emerg Infect Dis. 2006 Feb;12(2):274-9.
- Litvinov IV, St-Germain G, Pelletier R, Paradis M, Sheppard DC. Endemic human blastomycosis in Quebec, Canada, 1988-2011. Epidemiol Infect. 2013 Jun;141(6):1143-7.
- Cheikh Rouhou S, Racil H, Ismail O, Trabelsi S, Zarrouk M, Chaouch N, et al. Pulmonary blastomycosis: a case from Africa. ScientificWorldJournal. 2008 Nov 2;8:1098-103.
- Chakrabarti A, Slavin MA. Endemic fungal infections in the Asia-Pacific region. Med Mycol. 2011 May;49(4):337-44.
