Key points
- Clostridium tetani (C. tetani) bacteria produce potent toxins and can cause tetanus.
- C. tetani are common in the environment and infect people through breaks in the skin.
- Not being up to date with tetanus vaccines is the biggest risk factor for infection.
- Diagnostic tests aren’t useful in supporting or ruling out tetanus.
Cause
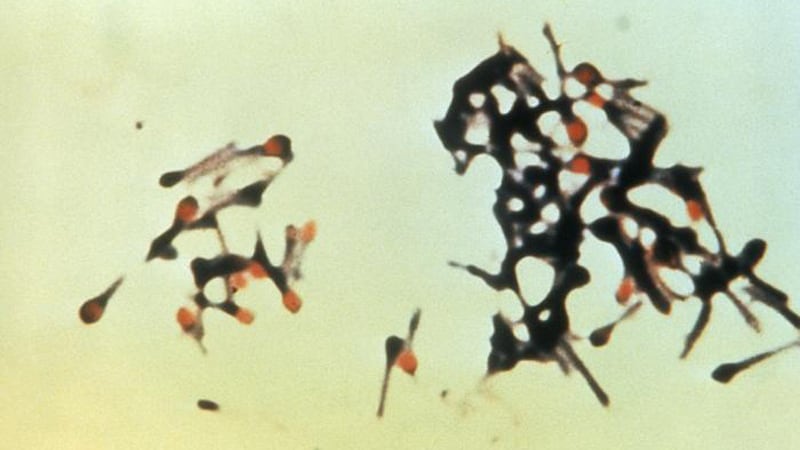
Tetanus is an infection caused by C. tetani spores. In anaerobic conditions, including those within the body, the spores germinate.
The bacteria produce very potent toxins that the blood stream and lymphatic system can disseminate throughout the body. One of these toxins, tetanospasmin (tetanus toxin), is responsible for the serious effects of tetanus.
Tetanus toxin
Tetanus toxin acts in the sympathetic nervous system and at several sites within the central nervous system:
- Brain
- Peripheral motor end plates
- Spinal cord
Tetanus toxin causes the typical clinical manifestations of tetanus by interfering with the release of neurotransmitters and blocking inhibitor impulses. This leads to unopposed muscle contraction and spasm.
Types
There are three clinical forms of tetanus: generalized (includes neonatal tetanus), localized, and cephalic. They present with different signs and symptoms.
Risk factors
Nearly all U.S. tetanus cases today are among adults who either
- Never received a tetanus vaccine
- Didn't stay up to date with their 10-year tetanus booster shots
Other risk factors for tetanus include:
- Being 70 years or older
- Having diabetes
- Immunosuppression
- Using intravenous drugs
Risk during natural disasters
Disasters such as earthquakes, hurricanes, floods, and tsunamis generally don't raise the level of tetanus in the environment.
However, the number of tetanus cases may increase during natural disasters because of injuries leading to tetanus exposure. There may also be delays in or lack of medical services and supplies.
Incubation period
Generalized and localized tetanus
The incubation period ranges from 3 to 21 days, averaging about 8 days.
In general, the further the injury site is from the central nervous system, the longer the incubation period. A shorter incubation period is associated with
- More severe disease
- Higher chance of death
Neonatal tetanus
Symptoms usually appear from 4 to 14 days after birth, averaging about 7 days.
Cephalic tetanus
The incubation period is short, usually 1 to 2 days.
How it spreads
C. tetani spores live in the environment. They usually enter the body through a wound or break in the skin.
Neonatal tetanus usually occurs when C. tetani enters the body after an umbilical stump infection.
Risk of death
Even with modern intensive care, generalized tetanus results in death for about 1 in 10 cases.
The risk of death from tetanus is highest among people 70 years of age or older.
Prevention
Wound management is a key strategy to prevent tetanus.
In addition, CDC recommends everyone stay up to date with their recommended tetanus vaccinations to prevent tetanus.
Diagnosis
CDC doesn't perform tetanus testing
Tetanus is a clinical syndrome. Healthcare providers diagnose tetanus based on clinical presentation, in the absence of a more likely cause. Clinical presentation of tetanus includes:
- Trismus (lockjaw)
- Spasms
- Muscle rigidity
- Difficulty swallowing or breathing (caused by muscle spasms)
- Other findings consistent with tetanus (e.g. rapid heart rate, extreme sweating)
Diagnostic tests aren’t useful in supporting or ruling out tetanus.
Surveillance and trends
Tetanus is an uncommon but reportable condition in the United States.
Resources
General
Tetanus chapter in the Vaccine-preventable Diseases Surveillance Manual
