Key points
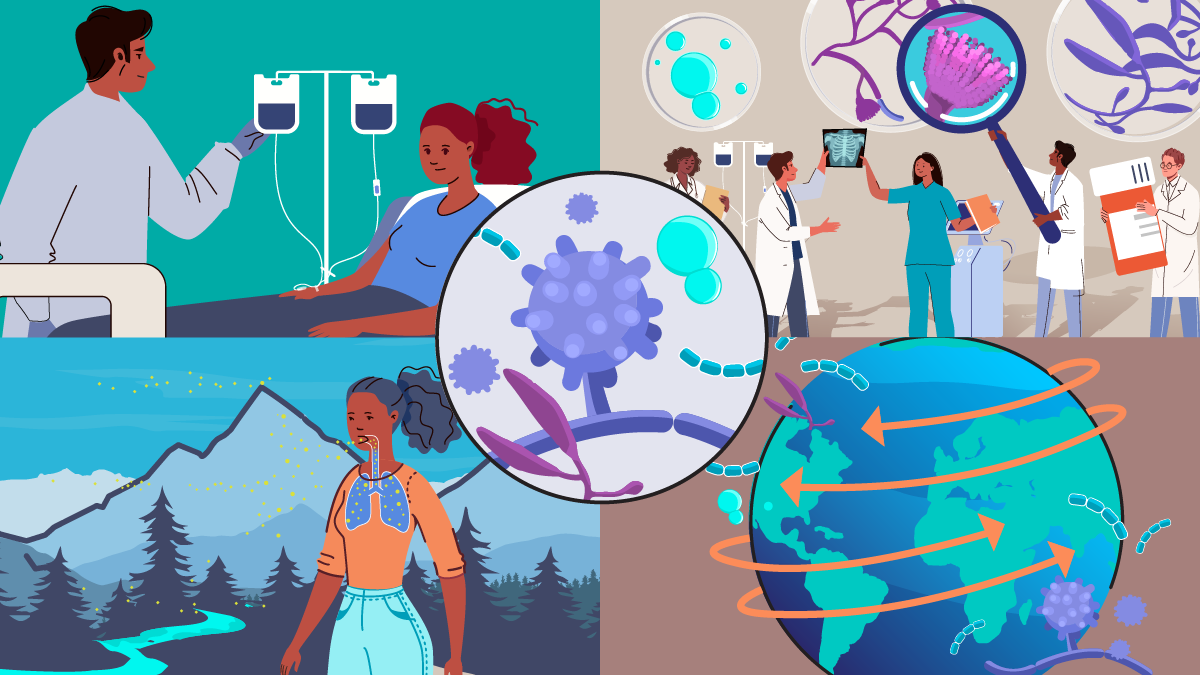
- Talaromycosis (formerly penicilliosis), a fungal infection, spreads in Southeast Asia, southern China, and India.
- Talaromycosis usually affects people with weakened immune systems.
- Bumps on the skin are common. Other symptoms vary and affect different parts of the body.
- Talaromycosis typically affects people with HIV differently than others who get infected.

Overview
Talaromycosis, formerly called penicillosis, is an infection caused by the fungus Talaromyces marneffei.
Talaromycosis affects people who live in or visit Southeast Asia, southern China, or northeastern India. Most people who get talaromycosis have a weakened immune system. People living with HIV are particularly at risk.
Skin bumps are a common sign of Tarlarmycosis. Other symptoms can include fever and cough. Talaromycosis usually affects people with HIV differently than other people who get infected.
Signs and symptoms
Most people who get talaromycosis already had a weakened immune system. Talarmycosis typically affects people with HIV differently than other people who get infected.
Common symptoms
Bumps on the skin are a common symptom. They are usually small and painless. The bumps usually appear on the face and neck but can also appear in other places on the body.
Other symptoms include:
- Fever
- General discomfort
- Weight loss
- Cough or shortness of breath
- Swollen lymph nodes, liver, or spleen
- Diarrhea
- Abdominal pain
The fungus can make people sick weeks to years after they come in contact with it.
Infections in people who have HIV
In people with advanced HIV disease, talaromycosis is more likely to spread to the bloodstream and other parts of the body. Skin bumps, fever and swelling of the spleen are also more common symptoms in people living with HIV. Skin bumps have a slightly different appearance and have a dent in the middle.
Infections in people who do not have HIV
Talaromycosis more commonly affects the mouth, throat, lungs, liver, and bone in people who do not have HIV. However it is still possible for infections to spread into the blood and other parts of hte body. Skin bumps are smooth without indentation in people with talaromycosis who do not have HIV.
Risk factors
Talaromycosis affects people who live in or visit Southeast Asia, southern China, or eastern India. Healthy people rarely get talaromycosis.
Most people who get talaromycosis have a medical condition that weakens their immune system, such as:
- Adult-onset immunodeficiency syndrome
- Cancer
- HIV/AIDS
- Organ transplant
- Other autoimmune diseases
Agricultural workers and farmers, particularly those working during the rainy season, appear to be more likely to get talaromycosis.

Thuy Le, M.D., D.Phil., Associate Professor, Duke University School of Medicine
Causes
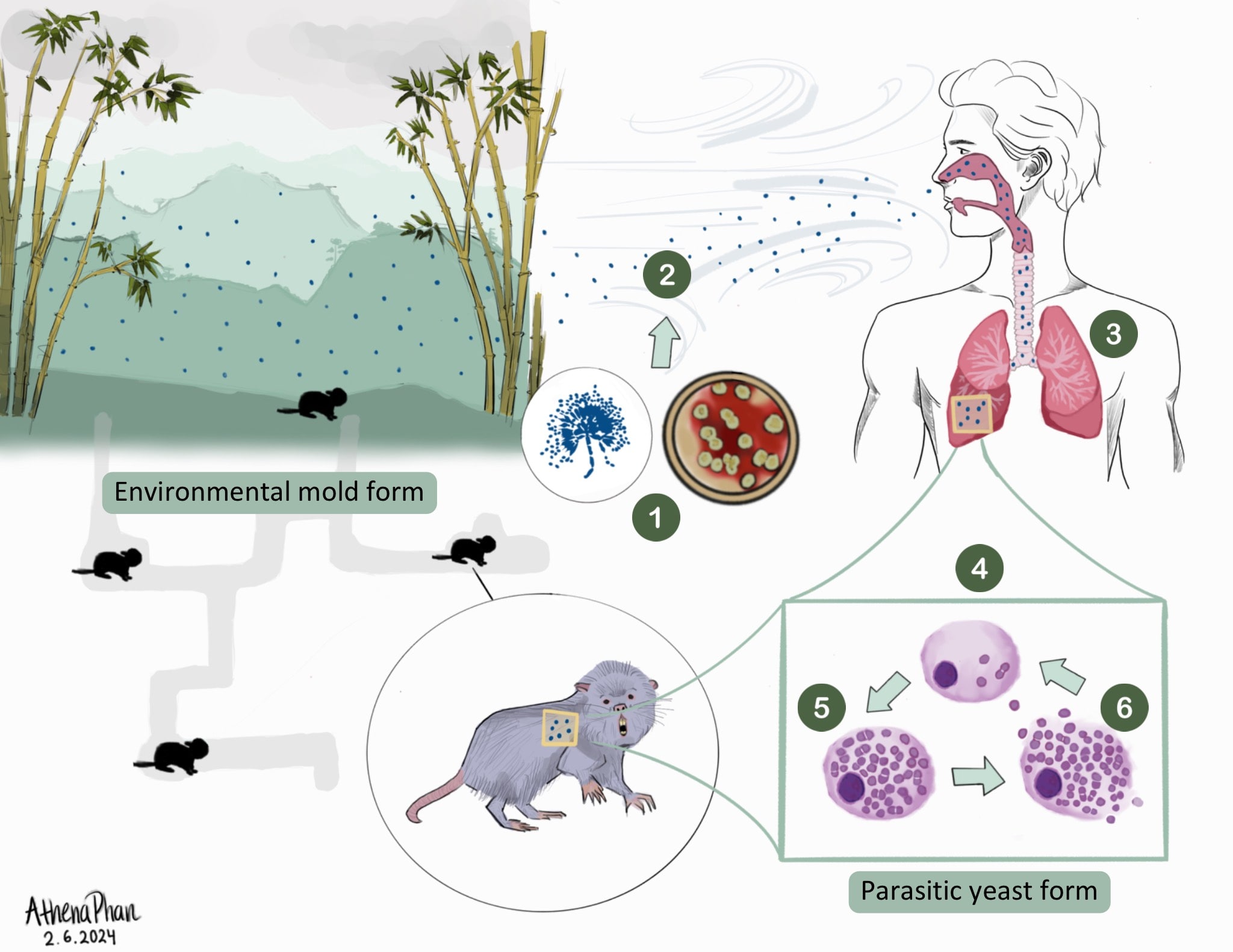
Scientitsts believe that people get talaromycosis after breathing in T. marneffei from the environment. Bamboo rats can also get talaromycosis but there is no evidence that it spreads from rats to people. Talaromycosis does not spread from person to person.
In Thailand, infections are more common during rainy seasons so rain might promote the growth of the fungus.
Talaromyces marneffei
Talaromyces marneffei can change from its native mold form in the environment to a parasitic yeast once in a warm-blooded host. In the environment (at 25°C), the mold form produces yellow green colonies and a characteristic soluble red pigment
Prevention
A healthcare provider might prescribe medicine to prevent talaromycosis in high-risk individuals. This includes people with weakened immune systems and who live in places where the fungus is present. Itraconazole is the most commonly used medicine to prevent talaromycosis. However, healthcare providers also can prescribe other antifungal medicines.
Testing and diagnosis
Talaromycosis can be diagnosed by using a sample from the body part that is affected. For example:
- Bone marrow
- Blood
- Fluid in and around the lungs
- Lymph node
- Skin
The sample is sent to a laboratory for a fungal culture or to be examined under the microscope. The sample can also be tested for the presence of a protein or DNA of the fungus.
Treatment and recovery
Talaromycosis must be treated with prescription antifungal medicine. The most common treatments are amphotericin B and itraconazole. Amphotericin B is given through a vein for two weeks, followed by itraconazole, given by mouth for 10 weeks. Other antifungal medicines that can be used include voriconazole or posaconazole.
More fungal disease resources
Communication and Educational Materials
Webinars, Podcasts, and Clinical Tools
- Vanittanakom N, Cooper CR, Jr., Fisher MC, Sirisanthana T. Penicillium marneffei infection and recent advances in the epidemiology and molecular biology aspectsexternal icon. Clin Microbiol Rev 2006;19:95-110.
- Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIVexternal icon. 2017
- Chan JF, Lau SK, Yuen KY, Woo PC. Talaromyces (Penicillium) marneffei infection in non-HIV-infected patientsexternal icon. Emerg Microbes Infect 2016;5:e19.
- Supparatpinyo K, Khamwan C, Baosoung V, Nelson KE, Sirisanthana T. Disseminated Penicillium marneffei infection in Southeast Asiaexternal icon. Lancet 1994;344:110-3.
- Wong SY, Wong KF. Penicillium marneffei infection in AIDSexternal icon. Patholog Res Int 2011;2011:764293.
- Kawila R, Chaiwarith R, Supparatpinyo K. Clinical and laboratory characteristics of Penicilliosis marneffei among patients with and without HIV infection in Northern Thailand: a retrospective studyexternal icon. BMC Infect Dis 2013;13:464.
- Bulterys PL, Le T, Quang VM, Nelson KE, Lloyd-Smith JO. Environmental predictors and incubation period of AIDS-associated Penicillium marneffei infection in Ho Chi Minh City, Vietnamexternal icon. Clin Infect Dis 2013;56:1273-9.
- Zheng J, Gui X, Cao Q, et al. A clinical study of acquired immunodeficiency syndrome associated Penicillium marneffei infection from a non-endemic area in Chinaexternal icon. PLoS One 2015;10:e0130376.
- Chariyalertsak S, Sirisanthana T, Supparatpinyo K, Praparattanapan J, Nelson KE. Case-control study of risk factors for Penicillium marneffei infection in human immunodeficiency virus-infected patients in northern Thailandexternal icon. Clin Infect Dis 1997;24:1080-6.
- Sirisanthana T. Penicillium marneffei infection in patients with AIDSexternal icon. Emerg Infect Dis 2001;7:561.
- Supparatpinyo K, Nelson KE, Merz WG, et al. Response to antifungal therapy by human immunodeficiency virus-infected patients with disseminated Penicillium marneffei infections and in vitro susceptibilities of isolates from clinical specimensexternal icon. Antimicrob Agents Chemother 1993;37:2407-11.