At a glance
- Sporotrichosis, caused by Sporothrix fungus, usually presents as a cutaneous infection.
- It is a considered a neglected tropical disease and causes devastating health and economic problems in some tropical and subtropical parts of the world.
- In the U.S., most infections are caused by the species Sporothrix schenckii (S. schenckii) that can be found in plant matter.
- In South America, the species Sporothrix brasiliensis (S. brasiliensis), transmitted by cats, is increasing.
- Sporotrichosis is best diagnosed by culturing clinical specimens.
- Treatment requires 3-6 months of oral antifungal medication. Severe infections may require intravenous antifungal treatment and cryosurgery.

Etiology
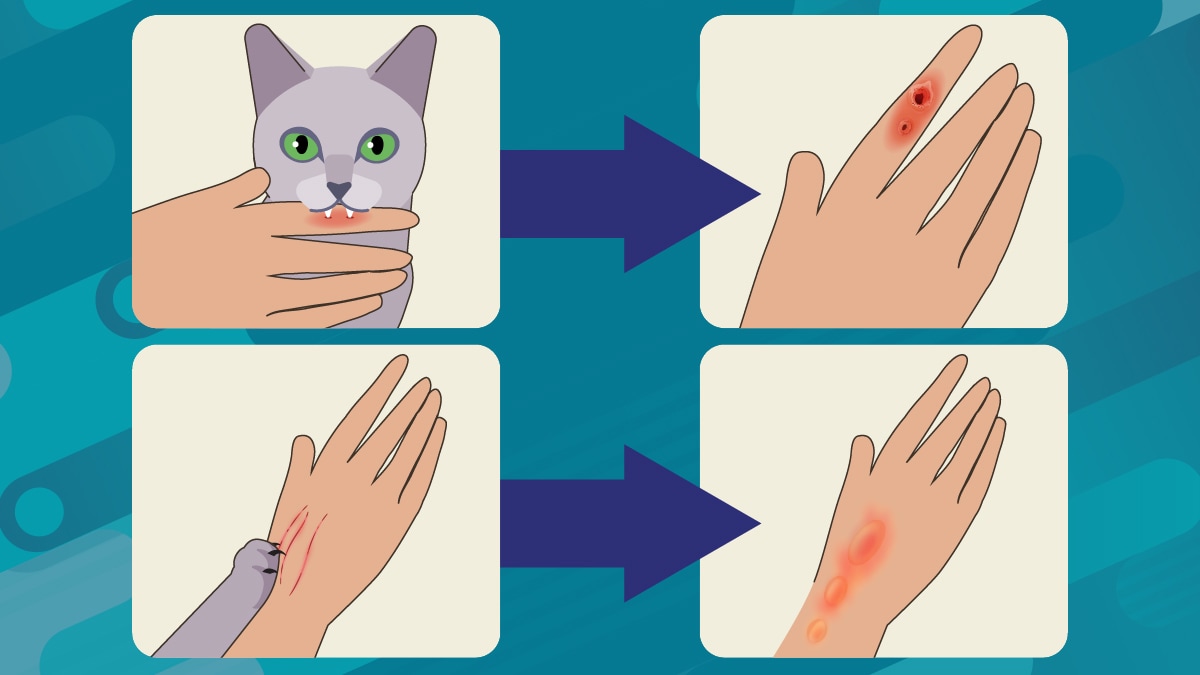
Sporothrix lives in soil and on plants, like sphagnum moss, rose bushes, and hay. People, cats, and other mammals can get sporotrichosis from exposure to Sporothrix. Infections are usually acquired through skin lacerations such as scrapes from thorns or plant matter or from bites or scratches from infected cats. It is sometimes referred to as "rose gardener's disease." Eye infections have been acquired, most likely through contact with respiratory droplets.
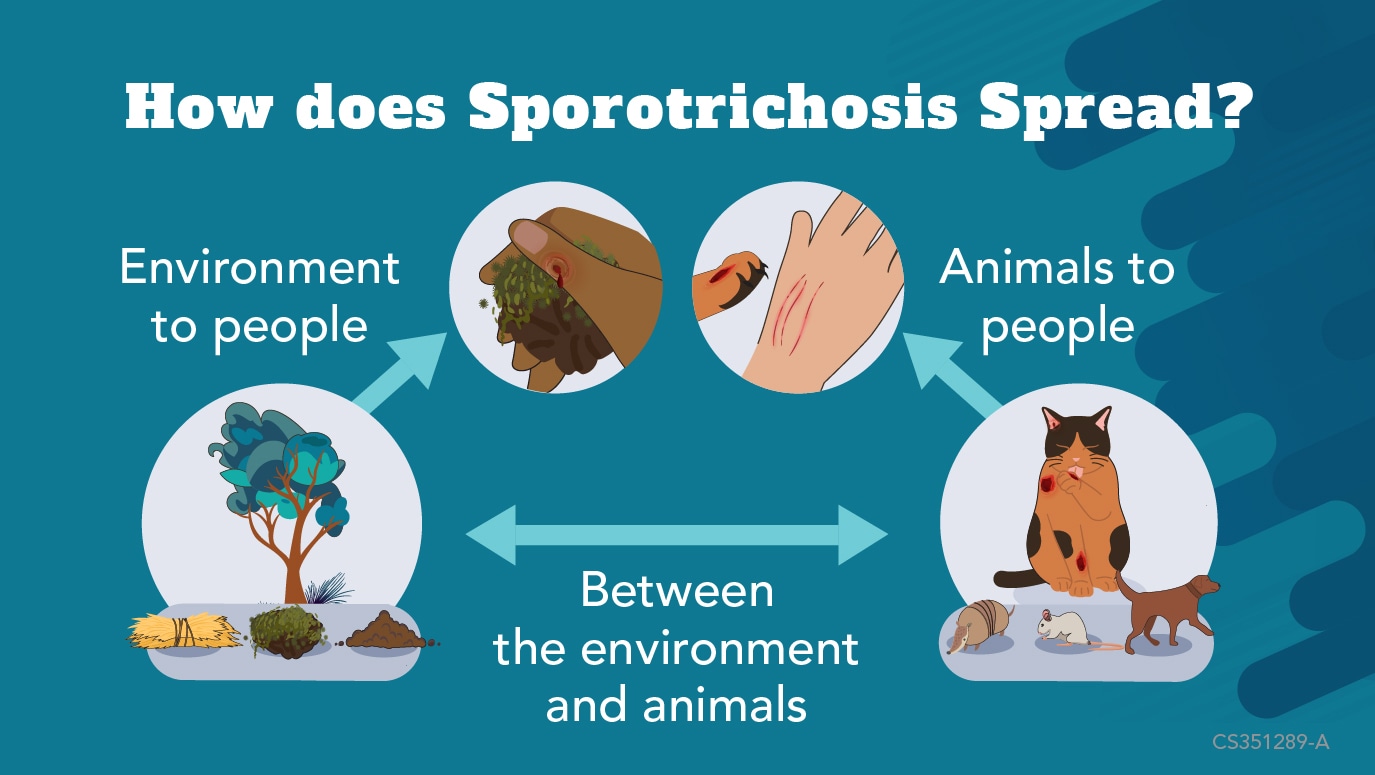
Sporothrix schenckii (S. schenckii) is the most common species in the United States and is typically transmitted through plant matter. Rarely, it can be transmitted to people from animals. Species that cause sporotrichosis in other parts of the world include S. brasiliensis, S. globosa and S. mexicana.
The species S. brasiliensis is increasingly spreading in parts of South America. It is primarily transmitted by cats and typically causes more severe symptoms.
More Information on Cat-associated Sporotrichosis
Clinical features
Human sporotrichosis is most often cutaneous. Less common it can cause extracutaneous or disseminated infections, particularly among people who are immunocompromised.
The cutaneous forms can cause:
- Subcutaneous nodules or abscesses
- Ulcerative lesions
- Enlarged lymph nodes
- Hypersensitivity reactions
The extracutaneous form and disseminated forms can cause:
- Ocular lesions
- Respiratory infections
- Pulmonary cavitation
- Bone invasion
- Encephalitis and meningitis
Prevention
Patients concerned about sporotrichosis should wear protective clothing, like gloves and long sleeves, when handling plant matter or hay.
Advise patients to avoid contact with cats with sores or wounds in areas with high rates of S. brasiliensis like South America.
Veterinary professionals should take precautions when examining cats, particularly in areas of high cat-to-human transmission. Currently cat-to-human transmission is rare in the United States. However, S. schenckii transmission from cat to veterinary staff has been reported. Veterinary professionals can take the following prevention measures:
- Wear examination gloves when handling cats with suspected infections.
- Take precautions to avoid scratches or bites.
- Wash any wounds from scratches or bites promptly with soap and water.
- Seek health care immediately if they develop skin lesions.
Diagnosis
Sporotrichosis is best diagnosed by a culture of clinical specimens. Molecular methods, such as polymerase chain reaction (PCR), can be used to determine the infecting species.
Cytology and immunohistochemistry can also be used for initial diagnosis. Serological tests for antibody detection are commercially available, but can vary in performance depending on the disease presentation.
Treatment and recovery
Sporotrichosis is typically treated with oral itraconazole. Supersaturated solution of potassium iodide (SSKI), posaconazole, terbinafine, and fluconazole are sometimes used. Amphotericin B may be required as initial therapy for severe disease. Prolonged treatment of 3–6 months or longer is often needed, depending on the type of infection and response to therapy. Cryosurgery may be considered for patients with thick keratotic skin lesions or who are pregnant.
Training for national and district-level health workers
Sporotrichosis: Training for national and district-level health (openwho.org)