Key points
- Mycoplasma pneumoniae are a common cause of bacterial respiratory infections.
- These bacteria have unique features that impact treatment options and pathogenesis.
- M. pneumoniae infections are most common in young adults and school-age children.
- In 2024, CDC has seen an increase in M. pneumoniae infections.

2024 increase
In October 2024, CDC issued a Bulletin about the increase in M. pneumoniae infections among children in the United States.
Cause
Exclusively a human pathogen, M. pneumoniae bacteria can cause respiratory tract infections.
Unique features
Of note, M. pneumoniae:
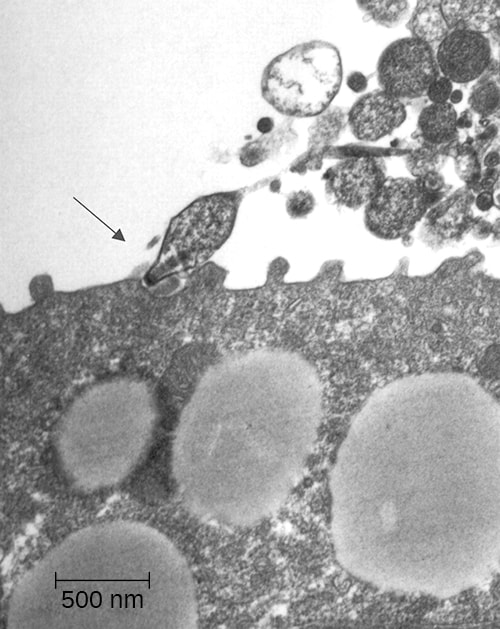
- Lack a rigid cell wall
- Associate closely with host cells
- Produce a toxin
- Can replicate intracellularly
Lack of cell wall impacts treatment options
Antimicrobials that target the cell wall (i.e., beta-lactam antibiotics) don't work against these bacteria.
Close association helps bacteria survive
A specialized attachment organelle allows close association with host cells. This prevents the host's mucociliary clearance mechanisms from removing the bacteria. It also activates the innate immune response and produces local cytotoxic effects.
Waites KB, Talkington DF. Mycoplasma pneumoniae and its role as a human pathogen. Clin Microbiol Rev. 2004;17:697–728.
Toxin production aids in colonization
A unique virulence factor, known as Community Acquired Respiratory Distress Syndrome (CARDS) toxin, likely aids in colonization. Experts believe it leads to inflammation and airway dysfunction.
Endocytosis offers unique challenges
While M. pneumoniae primarily live on the surface of respiratory epithelial cells, they can invade tissues. The endocytosis of M. pneumoniae by host cells could:
- Help establish a latent or chronic disease state
- Facilitate evasion of the host's immune response
- Interfere with efficacy of antibiotics
Types
M. pneumoniae infections can occur in the upper and lower respiratory tract.
Common manifestations include:
- Pharyngitis
- Pneumonia
- Tracheobronchitis
The bacteria can also cause a wide array of extrapulmonary manifestations without obvious respiratory disease.
Risk factors
M. pneumoniae infections can affect anyone, but age and crowded settings can increase risk.
Age
M. pneumoniae infections are most common in young adults and school-age children.
Crowded settings
People living and working in crowded settings are at increased risk, for example:
- College residence halls
- Detention or correctional facilities
- Hospitals
- Long-term care facilities
- Military training facilities
- Schools
Risk for severe infections
People at increased risk for serious infection include those
- Recovering from a respiratory illness
- With preexisting lung conditions (e.g., asthma, reactive airway disease)
- With a weakened immune system
Incubation period
The incubation period is generally between 1 to 4 weeks. Shorter and longer durations can occur.
Infection rates
There's no national reporting or surveillance system for M. pneumoniae infections. While common, the true number of people affected is unknown.
CDC can monitor national trends using syndromic and commercial laboratory data. In 2024, CDC has seen an increase in M. pneumoniae infections, including in young children.
Clinical features
People with a M. pneumoniae infection can have highly variable and non-specific presentations. Serious complications are uncommon but can occur.
Testing and diagnosis
The varied presentation and limited diagnostic methods available present unique challenges for accurately identifying M. pneumoniae cases and appropriately treating patients.
- Consider collecting respiratory specimens to test for M. pneumoniae along with other respiratory pathogens if there's increased respiratory illness in the community, especially among school-age children.
- Consider M. pneumoniae as a possible etiology among children hospitalized with community-acquired pneumonia.
- Have increased suspicion of M. pneumoniae among patients with community-acquired pneumonia who aren't clinically improving on antibiotics that are known to be ineffective against M. pneumoniae, such as beta-lactams.
- Perform laboratory testing when M. pneumoniae infection is suspected to ensure appropriate antibiotic therapy is administered, especially among hospitalized children.
- Consider swabbing both the throat and the nasopharynx to improve the likelihood of detection of M. pneumoniae in respiratory swab specimens. Adhere to proper specimen collection protocols.
Treatment and recovery
Most M. pneumoniae infections are self-limiting.
However, healthcare providers routinely treat pneumonia caused by M. pneumoniae with antibiotics.
