At a glance
CDC analyzed data from two large, nationally representative surveys to assess flu vaccination coverage for the 2023–24 flu season among children and adults in the United States.
Summary
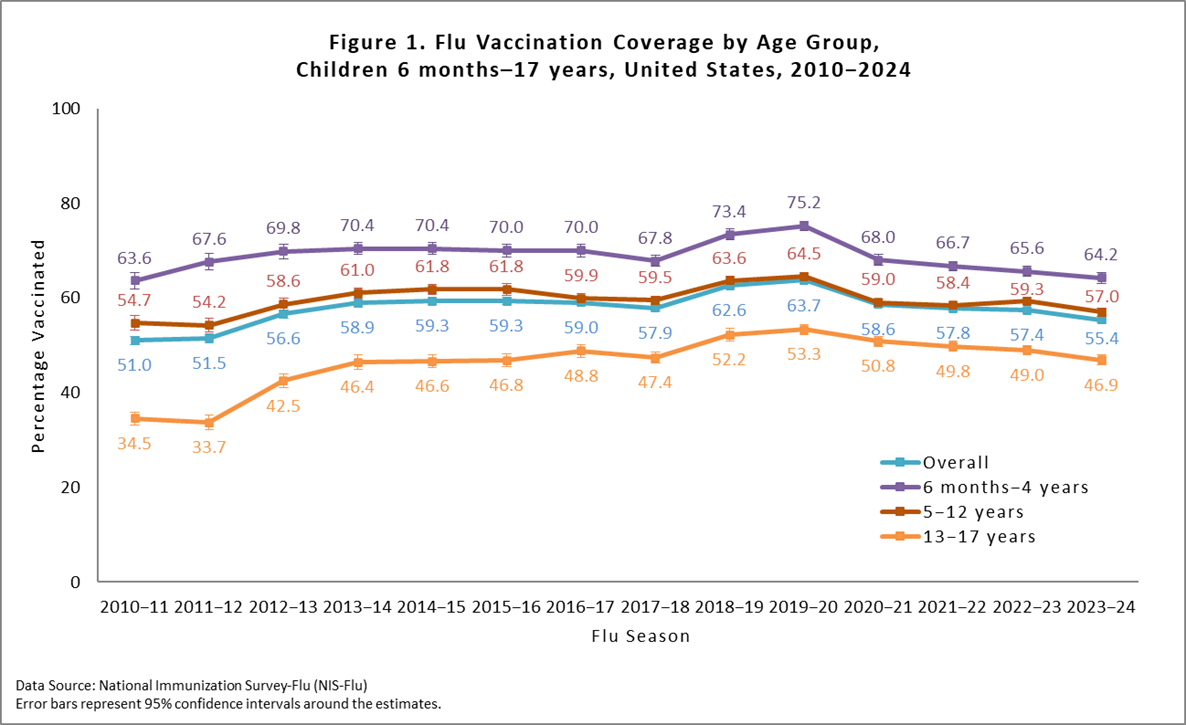
The Centers for Disease Control and Prevention (CDC) recommends annual influenza (flu) vaccination for all people ≥6 months who do not have contraindications1. To assess flu vaccination coverage for the 2023–24 flu season among children and adults in the United States, CDC analyzed data from two large, nationally representative surveys, the National Immunization Survey-Flu (NIS-Flu) and the Behavioral Risk Factor Surveillance System (BRFSS). This report contains CDC's final flu vaccination coverage estimates for the 2023–24 flu season. In the 2023–24 flu season, vaccination coverage with ≥1 dose of flu vaccine was 55.4% among children 6 months through 17 years, a decrease of 2.0 percentage points compared with the 2022–23 flu season (57.4%) and a decrease of 8.3 percentage points compared with the pre-pandemic 2019–20 season (63.7%). The last time flu vaccination coverage among children was this low or lower was 12 seasons ago (2011–12, 51.5%). Flu vaccination coverage among adults ≥18 years was 44.9%, a decrease of 2.0 percentage points from the prior season (46.9%). For adults, after an initial increase in flu vaccination coverage in the season immediately following the start of the COVID-19 pandemic, coverage has steadily declined since the 2020–21 season. The last time flu vaccination coverage among adults was lower was six seasons ago (2017–18, 37.1%). Interpretation of the estimates in this report should take into consideration survey limitations.
An annual flu vaccine is the best way to reduce the risk of illness and serious complications from flu. For most people, September and October are ideal times to get vaccinated; however, vaccination should continue after October as long as flu viruses are circulating and unexpired vaccine is available. CDC expects flu viruses to spread along with other viruses this fall and winter, including respiratory syncytial virus (RSV) and the virus that causes COVID-19, and recommends that people stay up-to-date on all vaccinations.
Methods
For this report, CDC analyzed data from the NIS-Flu for children 6 months through 17 years and the BRFSS for adults ≥18 years to estimate national- and state-level flu vaccination coverage for the 2023–24 flu season. The analyses included data collected from interviews completed from September 2023 for BRFSS and October 2023 for NIS-Flu through June 2024 for vaccinations received between July 1, 2023, and the time of interview or by May 31, 2024.
The NIS-Flu is a national random-digit-dialed cellular telephone survey of households2. Respondents ≥18 years knowledgeable about the child's vaccinations (hereafter referred to as "parent" in this report) were asked if their child received a flu vaccination since July 1, 2023, and the month of vaccination; this information was not verified by medical records. Month of vaccination was missing for 19.5% of respondents who indicated their child was vaccinated. For these children, month was imputed using the hot-deck imputation method from other survey respondents who matched the week of interview, age group, state of residence, and race/ethnicity of the child with missing data. Respondents who indicated the child received a flu vaccination were asked the place where the child was vaccinated. The range of the Council of American Survey and Research Organizations (CASRO) response rates for the NIS-Flu for the 2023–24 season was 21.8%–26.1%. The estimates for children are based on n=137,750 completed NIS-Flu interviews.
The BRFSS is a state-based random-digit-dialed cellular and landline telephone survey that collects information on various health conditions and risk behaviors from one randomly selected adult ≥18 years in a household. The BRFSS survey asks if the respondent has received a flu vaccine in the past 12 months and, if so, the month and year of vaccination3. For 9.1% of BRFSS participants who were vaccinated but had a missing month or year of vaccination, month and year were imputed using the hot-deck imputation method from other survey respondents who matched the week of the interview, age group, state of residence, and race/ethnicity of the respondent with missing data. Estimates are not available for the entire 2023–24 flu season for Arizona and Mississippi because interview data for January–June 2024 from these states were not available; therefore, estimates for these states represent vaccinations received only through November 2023 and not through May 2024 as for other states. The median state BRFSS response rate for a complete or partially complete interview was 44.2% for September–December 2023 and 43.5% for January–June 2024. The estimates for adults are based on n=306,822 completed BRFSS interviews.
Flu vaccination coverage estimates from both surveys were calculated using Kaplan-Meier survival analysis using the month of the reported flu vaccination to determine cumulative flu vaccination coverage. Coverage estimates for all persons ≥6 months were determined by combining the state-level monthly NIS-Flu and BRFSS estimates weighted by the age-specific populations of each state4. All estimates were weighted and analyzed using SAS and SAS-callable SUDAAN statistical software to account for the complex survey designs. Differences between groups and between 2023–24 and prior season (2022–23) estimates were determined using t-tests with significance at p<0.05. Increases or decreases noted in this report were statistically significant differences.
Results
Overall, the percentage of children receiving ≥1 dose of flu vaccine during the 2023–24 season was 55.4%. This was a decrease of 2.0 percentage points from the 2022–23 season (57.4%) and a decrease of 8.3 percentage points compared with the pre-pandemic 2019–20 season (63.7%, Figure 1). Flu vaccination coverage among children aged 6 months–4 years (64.2%) did not differ from coverage in the previous season, but coverage for children 5–12 years (57.0%), and 13–17 years (46.9%; Figure 1) had decreases of 2.3 and 2.1 percentage points, respectively, compared with the previous season. For additional results by age group, see the "Additional Flu Vaccination Coverage Estimates" section at the end of this report.
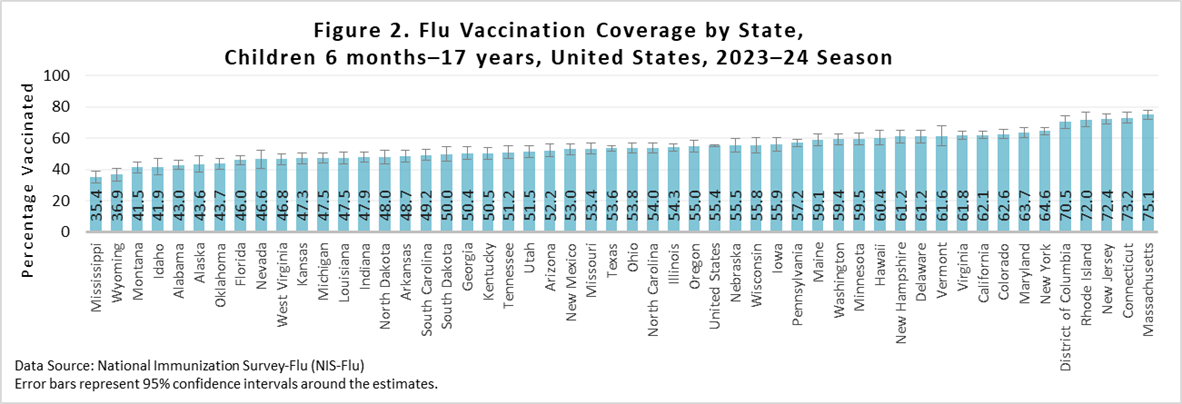
As is seen each flu season, there was wide (>39 percentage points) variability between states in flu vaccination coverage for children, ranging from 35.4% (Mississippi) to 75.1% (Massachusetts) (Figure 2). No jurisdictions had an increase in coverage this season compared with last season, while 13 had drops in coverage ranging from 2.7 to 10.8 percentage points. To view additional state-level final end of flu season vaccination coverage estimates using the same methods described in this report, see the interactive application at FluVaxView Interactive.
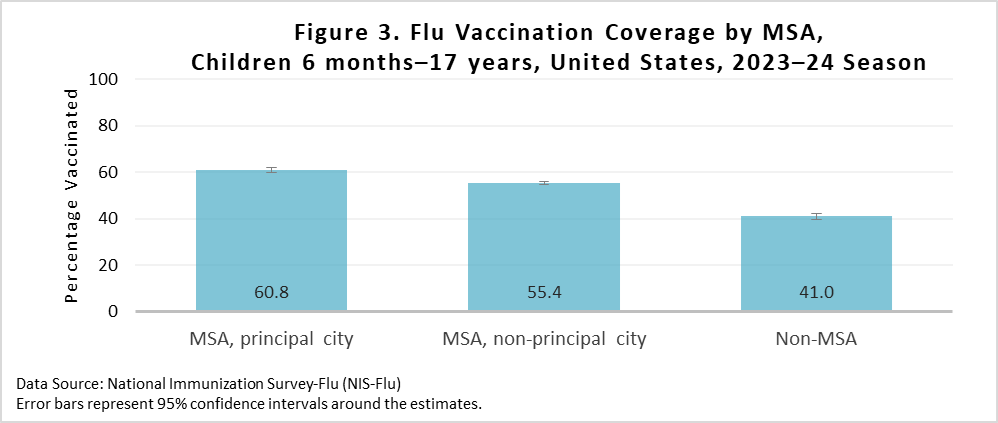
Vaccination coverage was higher for children living in a metropolitan statistical area (MSA) principal city (60.8%) compared with children living in a MSA non-principal city (55.4%) and children living in a non-MSA (41.0%) (Figure 3). Vaccination coverage was also higher for children living in a MSA non-principal city (55.4%) compared with children living in a non-MSA (41.0%). Additional results by MSA status are included in the "Additional Flu Vaccination Coverage Estimates" section of this report.
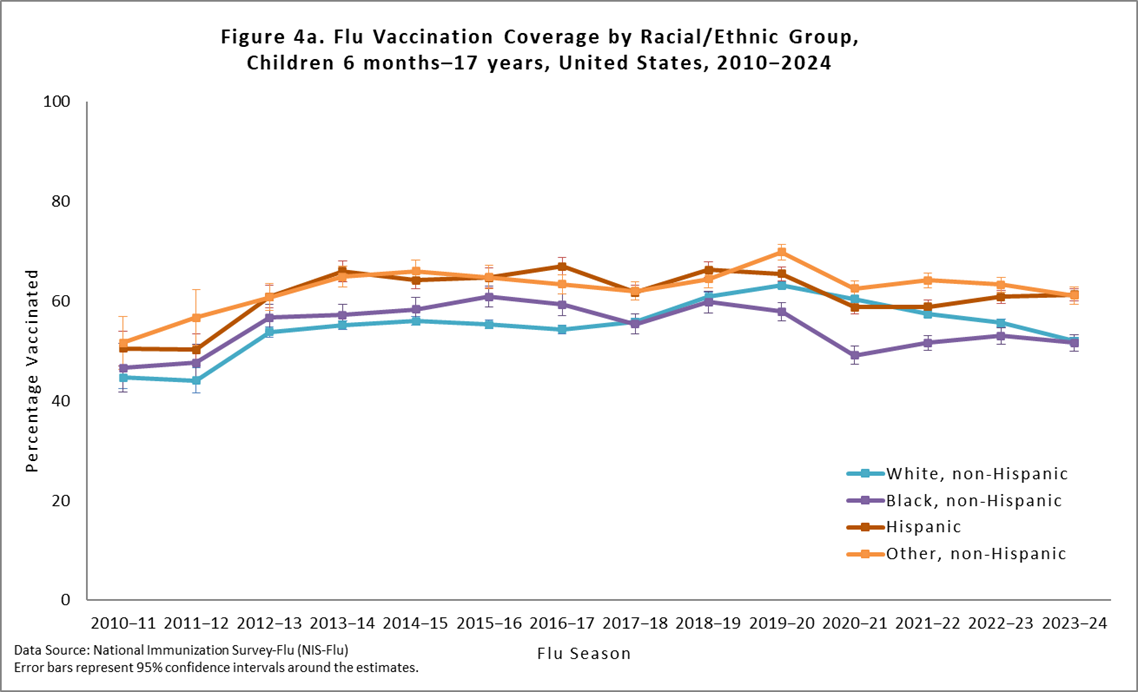
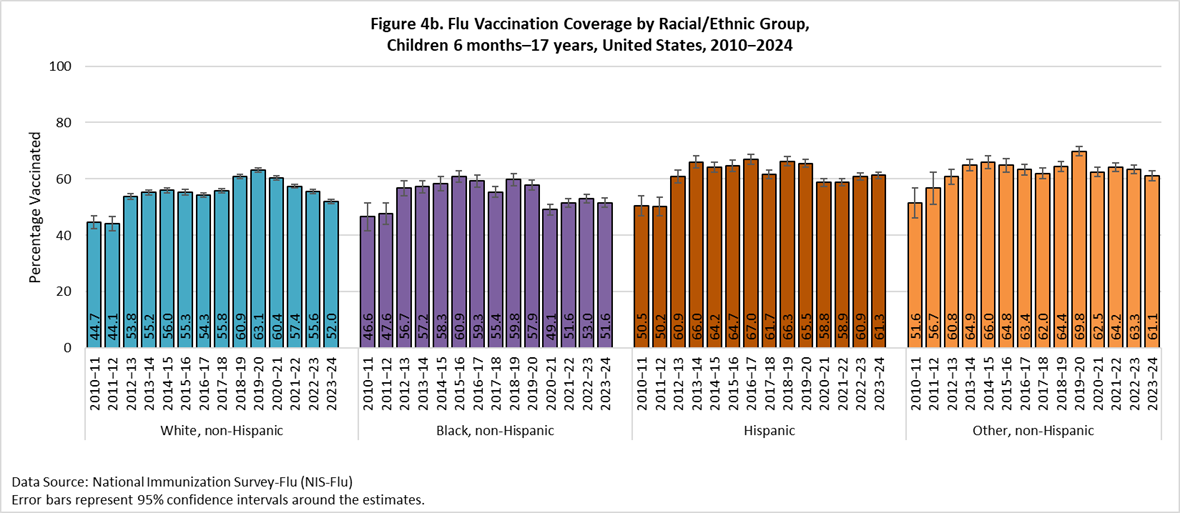
Flu vaccination coverage for the 2023–24 season decreased by 3.6 percentage points among non-Hispanic White (White) children compared with the 2022–23 season. Coverage for Hispanic, non-Hispanic Black (Black) children and non-Hispanic children of other or multiple races did not change compared with the previous season (Figures 4a and 4b). Hispanic children and non-Hispanic children of other/multiple races had higher flu vaccination coverage than Black children and White children. No other statistically significant pair-wise differences were observed. Flu vaccination coverage estimates for more detailed racial/ethnic groups (Asian, American Indian/Alaska Native) are provided as a table weblink in the "Additional Flu Vaccination Coverage Estimates" section of this report.
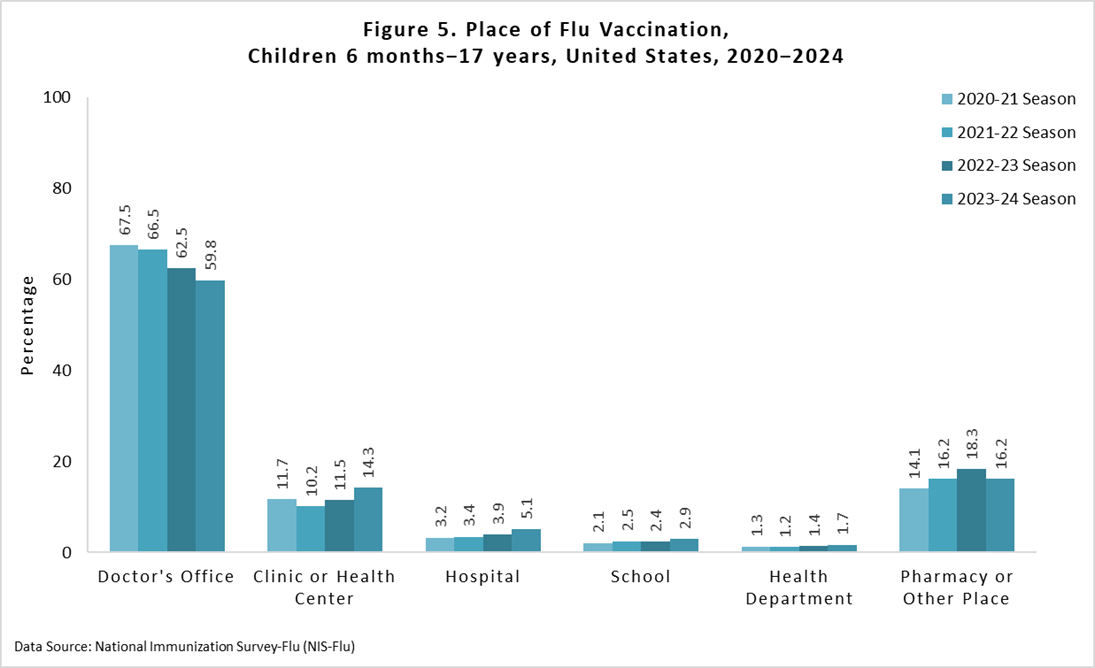
Place of flu vaccination among vaccinated children 6 months through 17 years for the 2023–24 season was most often a doctor's office (59.8%), followed by a pharmacy/other place (16.2%), and clinic/health center (14.3%) (Figure 5). Place of flu vaccination by child age groups can be found in the "Additional Flu Vaccination Coverage Estimates" section of this report.
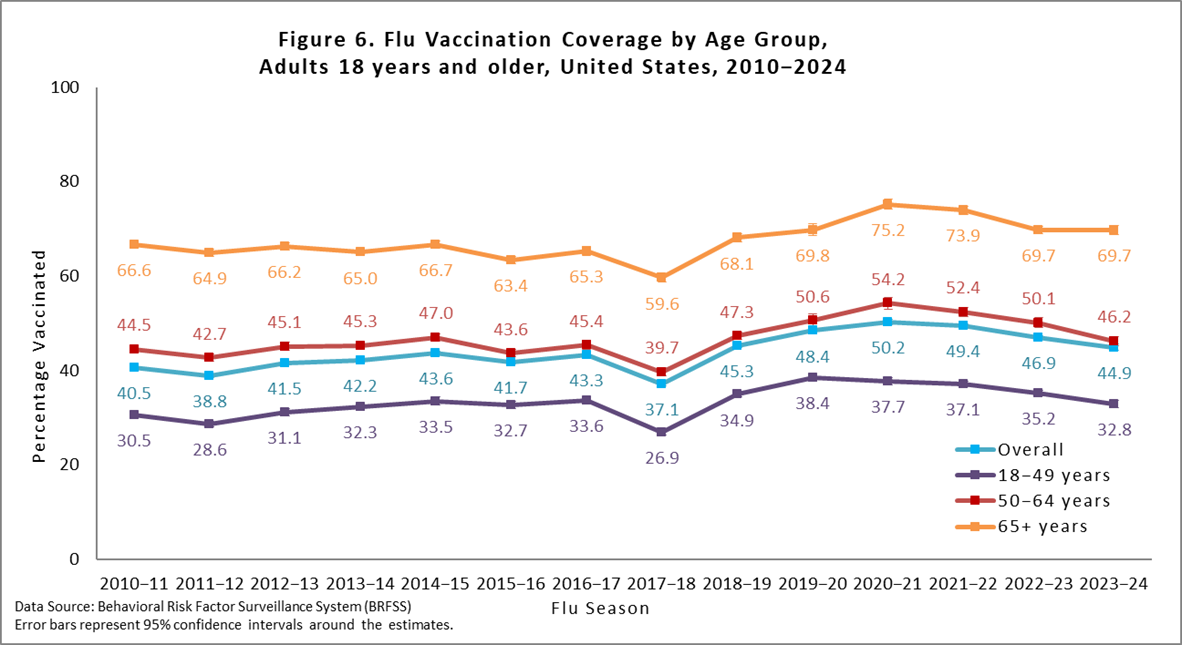
Overall, among adults ≥18 years, flu vaccination coverage was 44.9%, 2.0 percentage points lower than coverage during the 2022–23 season (46.9%; Figure 6). Compared with the 2022–23 season, flu vaccination coverage for 2023–24 was 2.4 percentage points lower among adults 18–49 years and 3.9 percentage points lower among adults 50–64 years, but similar to last season among adults ≥65 years (Figure 6).
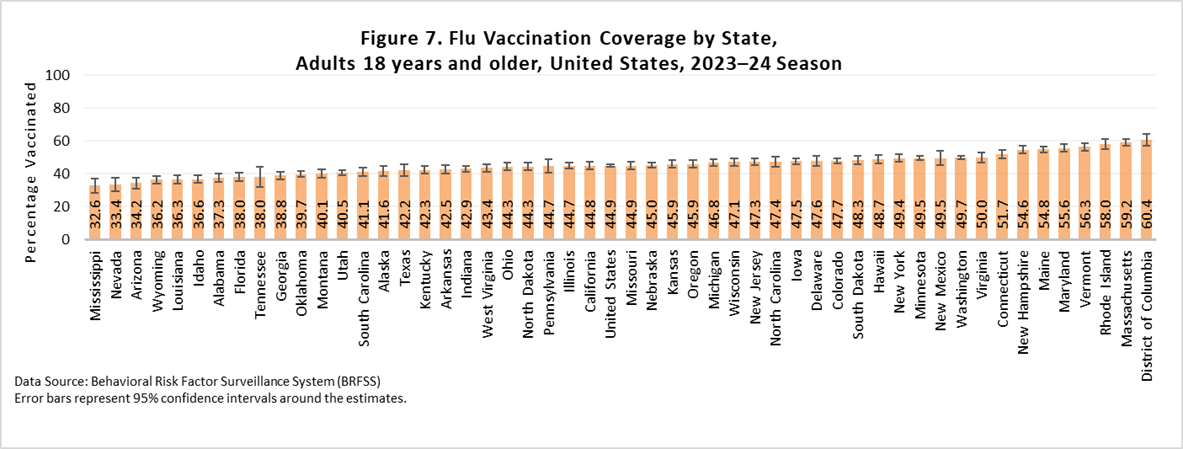
There was wide between-jurisdiction variability in flu vaccination coverage among adults, ranging from 32.6% in Mississippi to 60.4% in the District of Columbia (Figure 7). See FluVaxView Interactive General Population for additional state-level estimates by age-groups and multiple flu seasons. One state had an increase in coverage this season compared with last season, while 13 had drops in coverage ranging from 2.0 to 8.8 percentage points.
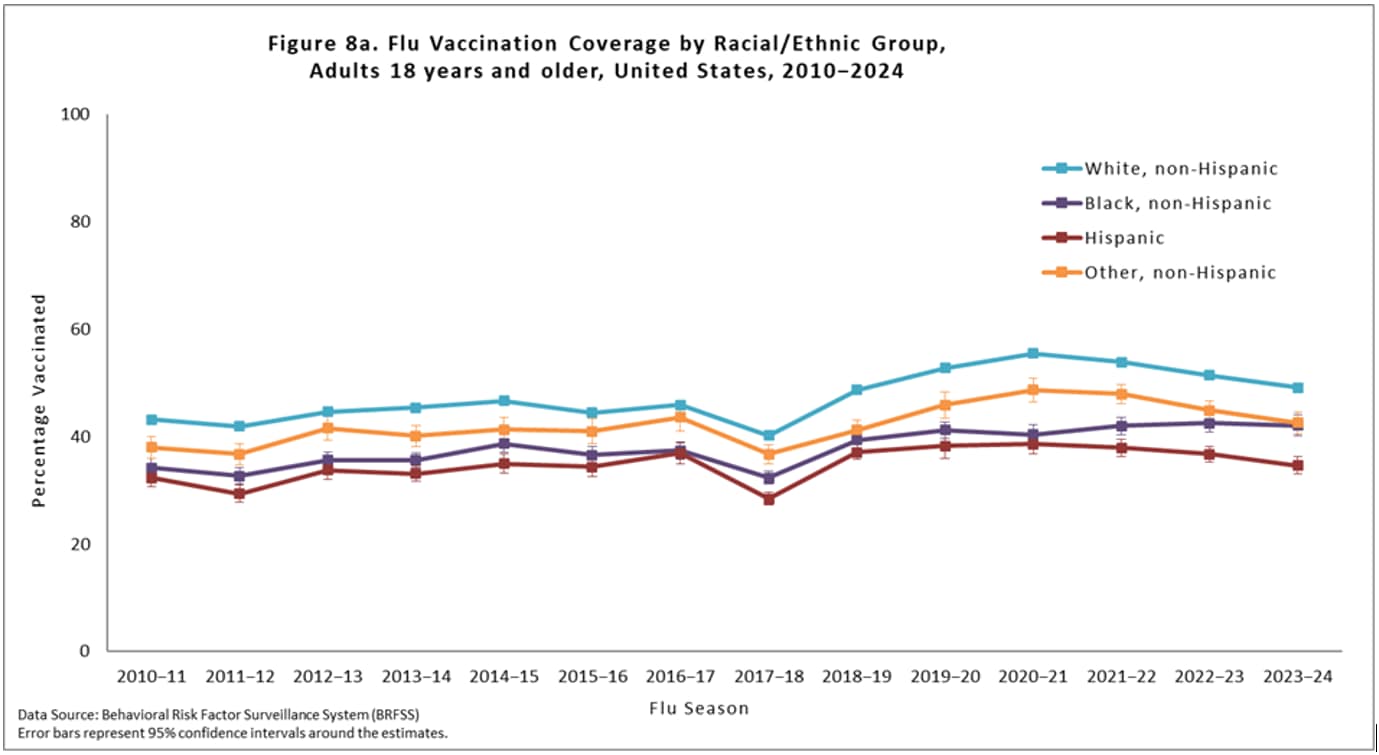
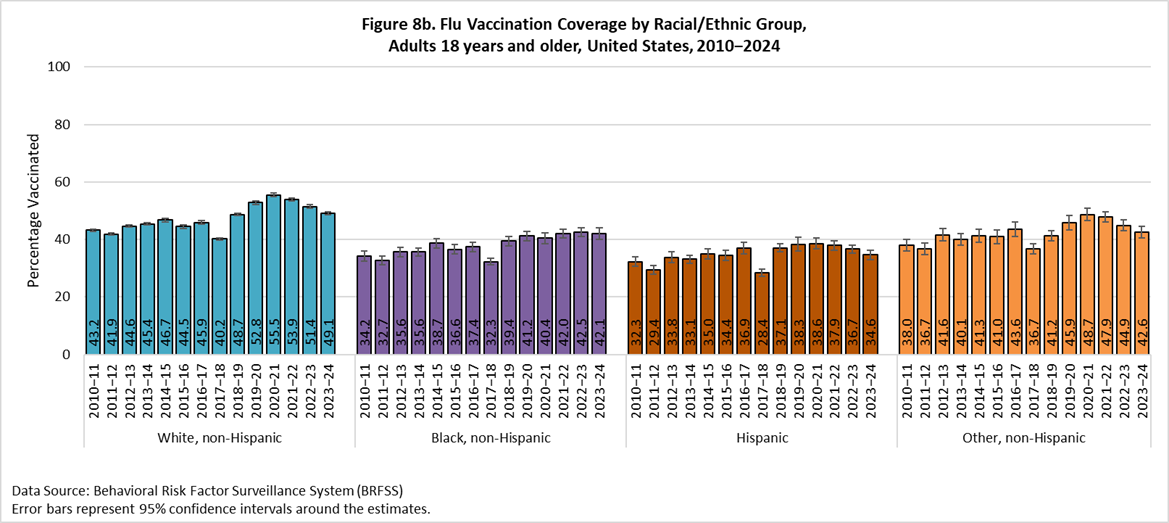
Flu vaccination coverage during the 2023–24 season for Black adults, Hispanic adults, and adults of other or multiple races did not differ compared with the 2022–23 season, while White adults had a 2.3 percentage point decrease in coverage (Figures 8a and 8b). White adults had higher flu vaccination coverage than Black, Hispanic, and adults of other or multiple races. Additionally, Hispanic adults had lower flu vaccination coverage than Black adults and adults of other or multiple races. No other differences were observed. Flu vaccination coverage estimates for more detailed racial/ethnic groups (Asian, American Indian/Alaska Native) are provided as a table weblink in the "Additional Flu Vaccination Coverage Estimates" section at the end of this report.
Flu vaccination coverage among all people ≥6 months during the 2023–24 season was 47.2%, 2.1 percentage points lower than coverage in the 2022–23 season (Table 1). Flu vaccination coverage during the 2023–24 season for Black people ≥6 months did not differ compared with the 2022–23 season, while White people ≥6 months had a 2.5 percentage point decrease in coverage, Hispanic people ≥6 months had a 1.6 percentage point decrease in coverage, and people of other or multiple races ≥6 months had a 2.5 percentage point decrease in coverage (Table 1). White people had higher flu coverage than Black, Hispanic, and people of other or multiple races. Additionally, people of other or multiple races had higher coverage than Black and Hispanic people and Black people had higher coverage than Hispanic people. No other differences were observed.
Table 1. Flu Vaccination Coverage* among All People 6 months and older, by Race/Ethnicity, United States, † 2023–24 Season
| Race/Ethnicity‡ | %§ ± 95% CI|| | Difference from the 2022–23 Season ± 95% CI |
|---|---|---|
| Overall | 47.2 ± 0.5 | -2.1 ± 0.6¶ |
| White only, non-Hispanic | 49.7 ± 0.5 | -2.5 ± 0.7¶ |
| Black only, non-Hispanic | 44.5 ± 1.5 | -0.6 ± 1.9 |
| Hispanic | 42.2 ± 1.2 | -1.6 ± 1.6¶ |
| Other or multiple races, non-Hispanic** | 47.1 ± 1.5 | -2.5 ± 2.1¶ |
* Estimates of the percentage vaccinated are based on interviews conducted September (BRFSS) or October (NIS-Flu) 2023 through June 2024 and reported vaccinations from July 2023 through May 2024.
† Excludes U.S. territories.
‡ Race is self-reported; people of Hispanic ethnicity may be of any race.
§ Percentage vaccinated. Percentages are weighted to the U.S. population. Month of vaccination was imputed for respondents with missing month of vaccination data.
|| Confidence interval (CI) half-widths.
¶ Statistically significant difference between the 2023–24 season and the 2022–23 season by t-test (p<0.05).
** Includes Asian, American Indian/Alaska Native, Native Hawaiian or other Pacific Islander, multiracial, and other races.
Children:
- Flu Vaccination Coverage, by Age Group, Children, United States, 2023–24 Season [XLS - 12 KB]
- Flu Vaccination Coverage by Sex, Children, United States, 2023–24 Season [XLS - 14 KB]
- Flu Vaccination Coverage by Race/Ethnicity and Age Group, Children, United States, 2023–24 Season [XLS - 15 KB]
- Flu Vaccination Coverage for Local Areas and Territories, Children, 2023–24 Season [XLS - 82 KB]
- Flu Vaccination Coverage by MSA, Children, United States, 2023–24 Season [XLS - 14 KB]
- Place of Flu Vaccination by Age Group, Children, United States, 2023–24 Season [XLS - 15 KB]
Adults:
- Flu Vaccination Coverage, by Age Group and High-Risk Status, Adults, United States, 2023–24 Season [XLS - 12 KB]
- Flu Vaccination Coverage by Sex, Adults, United States, 2023–24 Season [XLS - 14 KB]
- Flu Vaccination Coverage by Race/Ethnicity and Age Group, Adults, United States, 2023–24 Season [XLS - 16 KB]
- Flu Vaccination Coverage for Local Areas and Territories, Adults, 2023–24 Season [XLS - 45 KB]
- Comparison of BRFSS and NIS-ACM Flu Estimates, Adults, United States, 2023–24 Season [XLS - 18 KB]
Children and Adults:
Limitations
Several limitations of the estimates produced from the NIS-Flu and BRFSS surveys should be considered when interpreting the results in this report. First, survey weighting adjustments may not eliminate all the possible bias from incomplete sample frames; both surveys exclude households with no telephones, and NIS-Flu excludes households with only landline telephones. Second, response rates for both surveys were low, and flu vaccination coverage may differ between survey respondents and non-respondents; survey weighting adjustments may not adequately control these differences. Third, there may be misclassification of flu vaccination status due to recall errors of parents for NIS-Flu and of respondents for BRFSS56. A study published in 2020 found that parents over-reported flu vaccination by approximately 9 percentage points7. Fourth, errors from incomplete sample frame, nonresponse, and accuracy of reported flu vaccination status might change over time, leading to inaccurate assessment of trends in flu vaccination coverage. Fifth, due to BRFSS interview data not being available for all months from Arizona and Mississippi, estimates for these two states represent vaccination coverage through November rather than through May. Sixth, estimates based on the sources in this report have differed from National Health Interview Survey (NHIS) estimates8. NHIS, the data source for evaluating progress toward the Healthy People 2030 flu vaccination coverage objectives, uses a different sampling method than the NIS-Flu and BRFSS, and uses in-person interviews but also relies on self or parental report. A recent study found that NIS-Flu estimates were generally higher than NHIS estimates over several flu seasons for children8.
The final estimates in this report will differ from the preliminary, in-season estimates on CDC's Weekly Flu Vaccination Dashboard because of different surveys (for adults only [BRFSS vs NIS-Adult Covid Module (NIS-ACM)]), and different analytic approaches (Kaplan-Meier vs enhanced estimates). The weekly dashboard estimate for children at the end of May was 53.8%, whereas the final estimate included in this report is 55.4%; and for adults the dashboard estimate based on NIS-ACM was 47.9% whereas the final estimate included in this report based on BRFSS is 44.9%. CDC uses enhanced estimates produced weekly by the NIS contractor for the dashboards due to this method allowing for the production of weekly estimates in the absence of respondent-reported exact week of vaccination; Kaplan-Meir cannot be performed in this case because week of vaccination is not collected. Kaplan-Meier estimates are used for the final estimates in this report and utilize the reported month the vaccine was received. For children, the same data source is used for both the weekly dashboard and the final estimates, with the difference being only in the estimation method. For adults, the data source for the weekly dashboard is the NIS-ACM, for which weekly enhanced estimates can be calculated each week by the NIS contractor and the data source for the reports of final estimates is BRFSS, which has been used since at least the 2010–11 season. However, the data from BRFSS are not available until August following each season; thus, not allowing in-season routine monitoring of flu vaccination coverage. Comparisons of estimates from the different data sources are included in the "Additional Flu Vaccination Coverage Estimates" section of this report. CDC continues to assess consistency between flu vaccination coverage estimates from different surveys and other data sources and to evaluate the accuracy of estimates from these data sources.
Discussion
In the United States, flu vaccination coverage among children and adults continues to decline post-COVID-19 pandemic, most notably among White children and adults <65 years. During the 2023–24 season, approximately half of children and adults received a flu vaccination. The last flu season that coverage was lower than this season's level was 12 seasons ago for children and 6 seasons ago for adults. Before the COVID-19 pandemic, flu coverage had been slowly increasing. Downturns in coverage began during and after the pandemic. Flu vaccination levels have not rebounded to pre-pandemic levels and remain below the Healthy People 2030 national target of 70% for flu vaccination of persons ≥6 months.
For children, a 2023 study found that 30.9% of U.S. children had a parent hesitant about flu vaccines. This paper did not note any increase in parental flu hesitancy between 2020 and 2023, yet a flu hesitancy level of almost one third is quite high; by contrast, the percentage with a parent hesitant about vaccines such as measles, polio, and tetanus was 12.2%9. A national poll conducted in August 2024 found that 40% of adults said it is extremely important for parents to have their children vaccinated, which was a decrease from 58% when the question was asked in 2019 and from 64% in 2001, indicating a decrease over time in the importance placed on vaccinating children, at least among some groups of the U.S. population10. Coverage with other childhood vaccines, such as those required for school entry and human papillomavirus vaccination, have also decreased since the COVID-19 pandemic, though decreases were smaller than those seen for flu vaccination1112. The most commonly reported reasons parents have for not vaccinating their child against flu are concern about side effects/safety, belief that the flu vaccine does not work well, and belief that their child is unlikely to get very sick from flu, with <4% reporting cost or access as a reason for non-vaccination (CDC, unpublished conference presentation).
While flu vaccination coverage among adults ≥65 years is high (69.7%) and approaching the Healthy People 2030 goal of 70%, coverage among adults <65 years has been steadily decreasing. Data from another CDC survey showed that younger adults were more likely to have at least one issue or concern with flu vaccination than adults ≥65 years, with the most commonly reported issue being that they are not worried about getting the flu13. Based on recent publications, small declines have been seen for other adult vaccinations, such as pneumococcal vaccine and tetanus1415.
An annual seasonal flu vaccine is the best way to help reduce the risk of illness and serious complications from flu. For most people, September and October are ideal times to get vaccinated. However, flu vaccination should continue throughout the flu season as long as flu viruses are circulating. To avoid missed opportunities for vaccination, the Standards for Adult Immunization Practice recommends that all providers routinely assess individuals' vaccination status at every clinical encounter, that they strongly recommend approved vaccinations to their patients, either offer needed vaccines or refer their patients to another provider who can administer the needed vaccines, and document vaccinations received by their patients in an immunization information system16. CDC expects flu viruses to spread along with other viruses this fall and winter, including RSV and the virus that causes COVID-19, and recommends that people stay up-to-date on all vaccinations.
- Grohskopf, L.A., et al., Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices - United States, 2024-25 Influenza Season. MMWR Recomm Rep, 2024. 73(5): p. 1-25.
- Wolter, K.K., et al., Statistical Methodology of the National Immunization Survey, 2005-2014. Vital Health Stat 1, 2017(61): p. 1-107.
- CDC. The BRFSS Data User Guide. 2013; Available from: https://www.cdc.gov/brfss/data_documentation/pdf/UserguideJune2013.pdf.
- Furlow-Parmley, C., et al., Combining estimates from two surveys: an example from monitoring 2009 influenza A (H1N1) pandemic vaccination. Stat Med, 2012. 31(27): p. 3285-94.
- Brown, C., et al., Validity of parental report of influenza vaccination in young children seeking medical care. Vaccine, 2011. 29(51): p. 9488-92.
- Irving, S.A., et al., Evaluation of self-reported and registry-based influenza vaccination status in a Wisconsin cohort. Vaccine, 2009. 27(47): p. 6546-9.
- Ogokeh, C.E., et al., Comparison of Parental Report of Influenza Vaccination to Documented Records in Children Hospitalized With Acute Respiratory Illness, 2015-2016. J Pediatric Infect Dis Soc, 2021. 10(4): p. 389-397.
- Santibanez, T.A., et al., Trends in Childhood Influenza Vaccination Coverage, United States, 2012-2019. Public Health Rep, 2020. 135(5): p. 640-649.
- Santibanez, T.A., et al., Parental hesitancy about COVID-19, influenza, HPV, and other childhood vaccines. Vaccine, 2024.
- Gallup. Far fewer in U.S. regard childhood vaccinations as important. 2024; Available from: https://news.gallup.com/poll/648308/far-fewer-regard-childhood-vaccinations-important.aspx.
- Pingali, C., et al., Vaccination Coverage Among Adolescents Aged 13-17 Years - National Immunization Survey-Teen, United States, 2022. MMWR Morb Mortal Wkly Rep, 2023. 72(34): p. 912-919.
- Seither, R., et al., Coverage with Selected Vaccines and Exemption from School Vaccine Requirements Among Children in Kindergarten - United States, 2022-23 School Year. MMWR Morb Mortal Wkly Rep, 2023. 72(45): p. 1217-1224.
- CDC. Results from omnibus surveys on vaccination receipt, intent, and knowledge, attitudes, beliefs, and behaviors, January 2024. 2024; Available from: https://www.cdc.gov/vaccines/ed/downloads/omnibus-vaccination-surveys-2024-01.pdf.
- CDC. Vaccination Coverage among Adults in the United States, National Health Interview Survey, 2022. 2024; Available from: https://www.cdc.gov/vaccines/imz-managers/coverage/adultvaxview/pubs-resources/vaccination-coverage-adults-2022.html.
- CDC. AdultVaxView:Vaccination coverage among adults. 2024; Available from: https://www.cdc.gov/vaccines/imz-managers/coverage/adultvaxview/data-reports/general-population/index.html.
- Recommendations from the National Vaccine Advisory committee: standards for adult immunization practice. Public Health Rep, 2014. 129(2): p. 115-23.
