At a glance
- Chromoblastomycosis is an implantation fungal infection caused by melanized, dematiaceous fungi that live in soil and on wood and plants.
- It most often occurs in tropical and subtropical regions, but cases have been reported in the United States.
- Lesions may resemble other infectious or non-infectious skin lesions.
- Without treatment, chromoblastomycosis can cause limb swelling, difficulty walking, skin cancer, and scarring of the skin.
- These physical effects can lead to social stigma.

Etiology
Chromoblastomycosis occurs when a break in the skin allows fungi to enter. It is caused by melanized, dematiaceous (black) fungi.
Reservoir and endemic areas
These fungi are associated with certain plants (e.g., thorns of Mimosa plant, Madagascar palm house plant, babassu coconut). Some species are more common in certain climates. For example, F. pedrosoi and F. nubica infections are commonly acquired in tropical regions, while C. carrionii infections are more commonly acquired in semiarid regions.
Types
The most common causes of chromoblastomycosis are Fonsecaea pedrosoi, F. monophora, F. nubica, Cladophialophora carrionii, Rhinocladiella aquaspersa, and Phialophora verrucosa. However, species distribution varies by region and climatic conditions.
Risk factors
Chromoblastomycosis can affect immunocompetent and immunocompromised individuals including people who are malnourished. It is more common in people who work or perform activities outdoors (e.g., farmers, gardeners, forestry workers, vendors of farm products).
Lack of protective gear (e.g. shoes, gloves), poor hygiene, and inadequate nutrition may increase the chance of getting chromoblastomycosis.
Clinical features
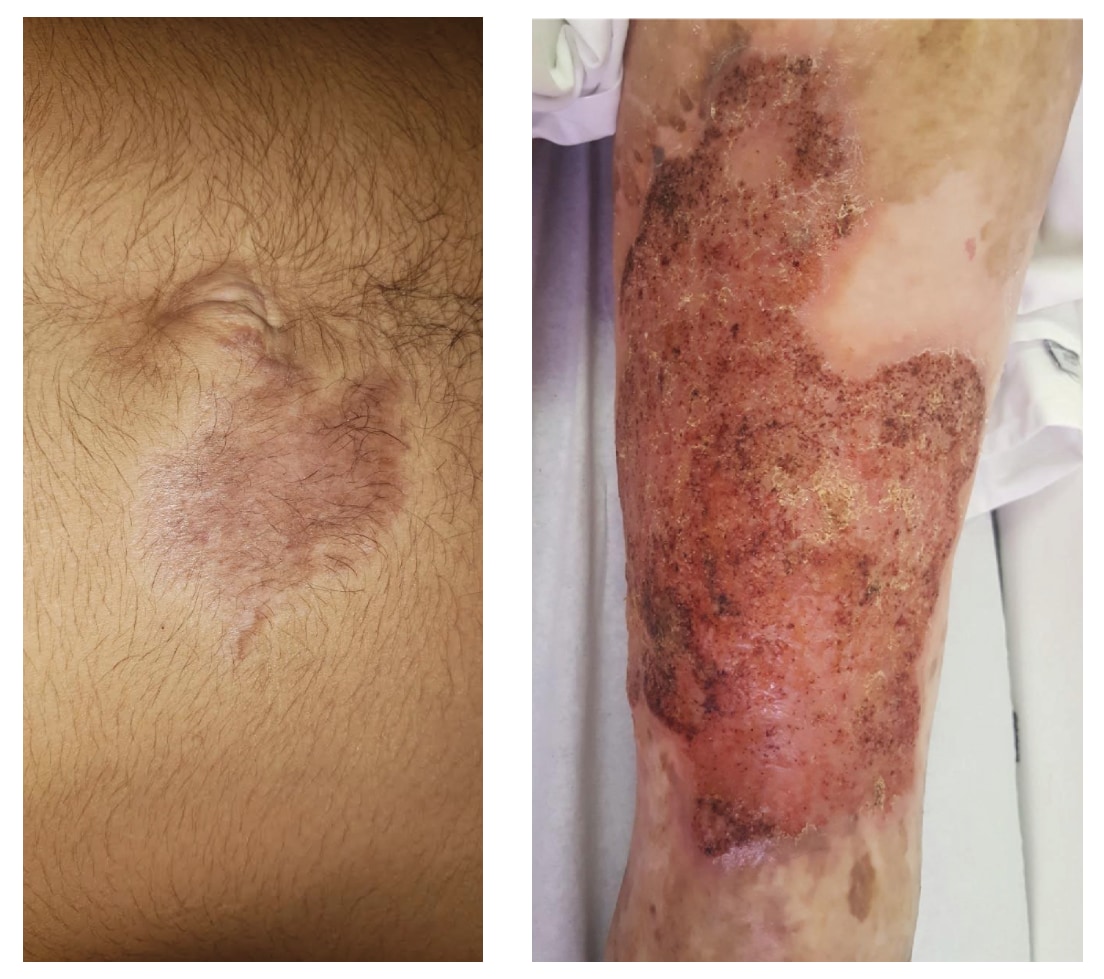
Chromoblastomycosis is a chronic progressive fungal infection of the skin and subcutaneous tissue. Most infections present on the lower or upper limbs, but infections can occur anywhere on the body. Typically, the infection first presents as erythematous papules (sometimes macules) at the site of inoculation.
Over time, these lesions may progress covering larger areas of the skin with nodular, verrucous, tumoral, plaque, or scar-like morphologies. Chromoblastomycosis progresses slowly over months to years. If left untreated can cause lymphedema, secondary bacterial infections, squamous cell carcinoma, tissue fibrosis, difficulty walking, and social stigma.
Prevention
Using personal protective equipment (e.g., gloves, shoes, appropriate clothing) and water, sanitation, and hygiene (WASH) may help prevent infections.
There are no available vaccines for chromoblastomycosis.
Early diagnosis and treatment can prevent severe disease, disability, and long-term complications.
Diagnosis
Diagnosis starts with obtaining skin scrapings from lesions or a skin biopsy. Confirming chromoblastomycosis depends on visualizing microscopically the characteristic thick-walled, single, or multicellular clusters of pigmented fungal cells. These fungal cells, often with pigmented internal cross walls, resemble copper pennies. These are also known as 'medlar bodies', 'muriform cells', or 'sclerotic bodies.'
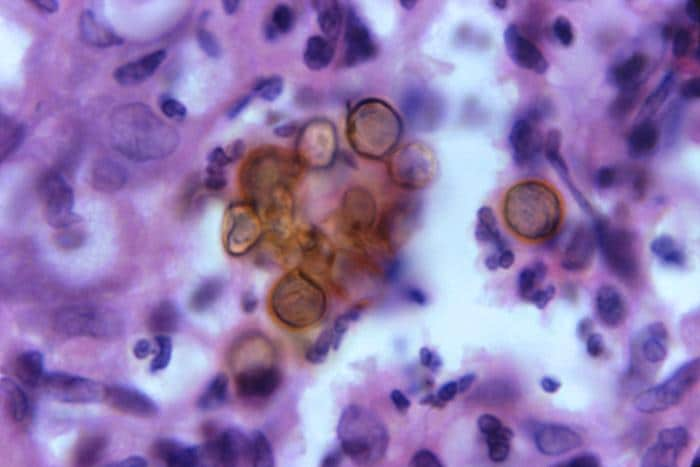
Clusters of these cells can be found in the dark spots seen on the surface of the skin lesions. These provide the best sites for taking a skin scraping with a scalpel blade or for a biopsy.
Microscopy: Examination of skin scrapings through direct microscopy with a potassium hydroxide (KOH) mount can identify these characteristic pigmented fungal cells.
Histopathology: Examination of a skin biopsy can find the presence of pigmented fungal cells in the dermis.
Culture and molecular diagnosis: Helpful in confirming the diagnosis. Decisions on treatment can be made without identification of the organism. Fungi that cause chromoblastomycosis are slow-growing and can take weeks before growing by culture.
There are no commercially available serologic tests available.
Treatment and recovery
Global guidelines are not available for treatment of chromoblastomycosis. Prolonged oral therapy (months to years) is often required. Itraconazole is typically considered first-line therapy with cure rates ranging from 15–80%.
Terbinafine is also frequently used to treat chromoblastomycosis. It may offer advantages over itraconazole such as better absorption and fewer drug-drug interactions.
Other triazole agents such as voriconazole and posaconazole have been reported to have favorable clinical response in refractory disease. Combination therapy with itraconazole and terbinafine or 5-flucytosine have been used in clinical practice for severe or refractory disease.
There is no evidence that different fungal species respond differently to the antifungal medicines recommended for treatment.
Other methods of treatment include topical immune response modulators, local application of heat, cryotherapy, and photodynamic therapy.
Treatment Access
Surveillance and Statistics
Chromoblastomycosis is designated as a neglected tropical disease by the World Health Organization. Chromoblastomycosis is not reportable in any U.S. jurisdiction or in most countries globally. Reliable disease burden estimates are lacking due to absence of national, regional, or global disease surveillance systems or networks. However, some researchers estimate the global burden to be greater than 7,000 cases, but this is likely a substantial underestimation.
The Global Chromoblastomycosis Working Group is a multidisciplinary team dedicated to controlling this implantation mycosis and encourages anyone interested to join.
