At a glance
As of November 18, 2024
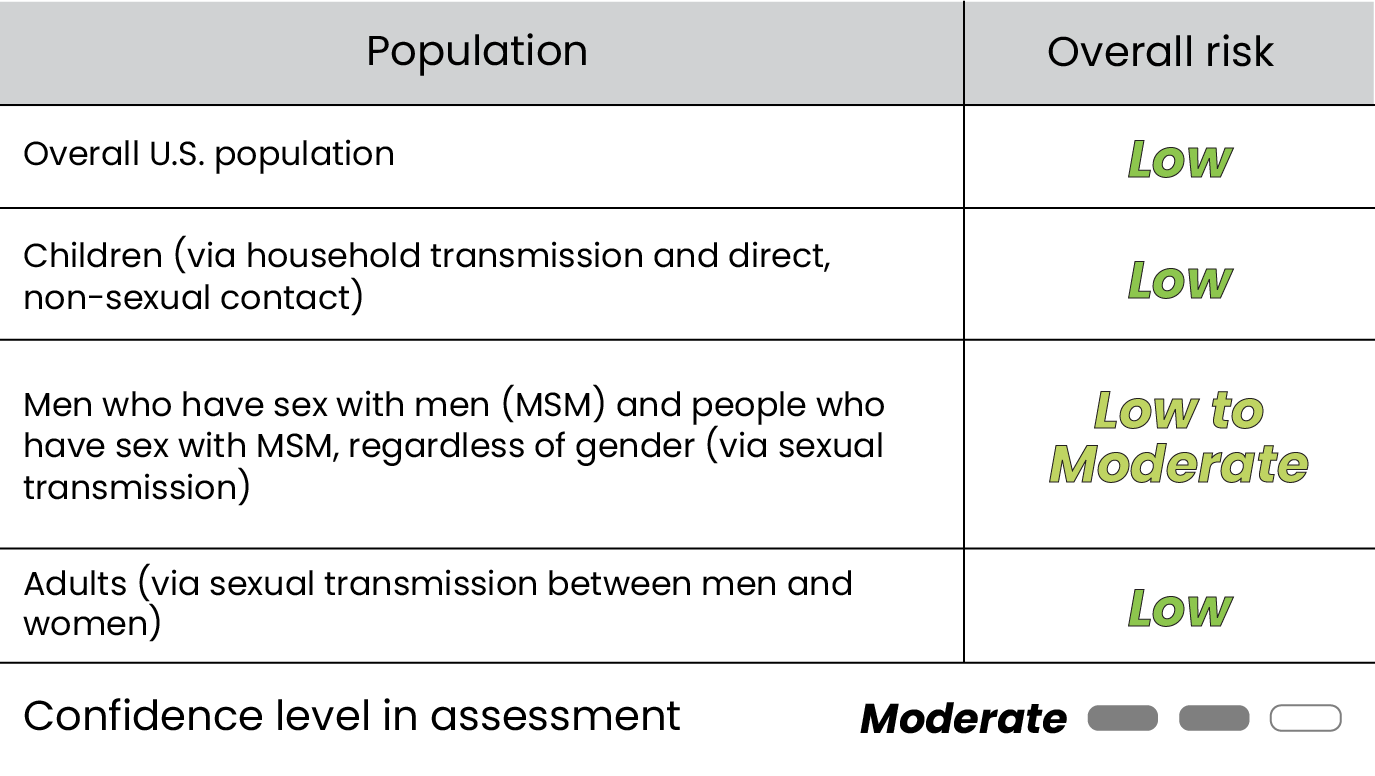
CDC assessed the risk to the United States overall population and specific populations within the United States posed by the clade I mpox outbreak in the Democratic Republic of the Congo (DRC) and in countries in Central and Eastern Africa:
The purpose of this assessment is to provide context about the ongoing outbreak of clade I mpox in DRC and in countries in Central and Eastern Africa, to inform U.S. preparedness efforts.
This assessment is an update to our August 30, 2024 risk assessment, incorporating new evidence and breaking out specific populations at risk. We note that the overall U.S. population includes the specific populations assessed, but we include specific populations separately because the clade I mpox outbreak in DRC and in countries in Central and Eastern Africa may pose higher risks to these populations. We chose these specific populations based on the most common mpox transmission routes for both the current clade I outbreak and the clade IIb outbreak that began in 2022.
We assessed overall risk by considering both likelihood and impact of infection in each population (see Methods section), under the assumption that a clade I mpox case was introduced into each population of interest. Both the likelihood and impact of infection are assessed at a population level. Likelihood of infection considers factors such as pathogen infectiousness and population susceptibility, while impact of infection considers factors such as disease severity, treatment availability, and public health response resources.
As of November 18, 2024, we are aware of the first case of clade I mpox in the United States. We assess risk to each population under the assumption that a clade I mpox case is introduced to these same populations; given there has been no spread beyond this case to date, this assessment does not change.
We continue to monitor the outbreaks of clade I mpox in Central and Eastern Africa and will update this risk assessment if new information warrants changes.
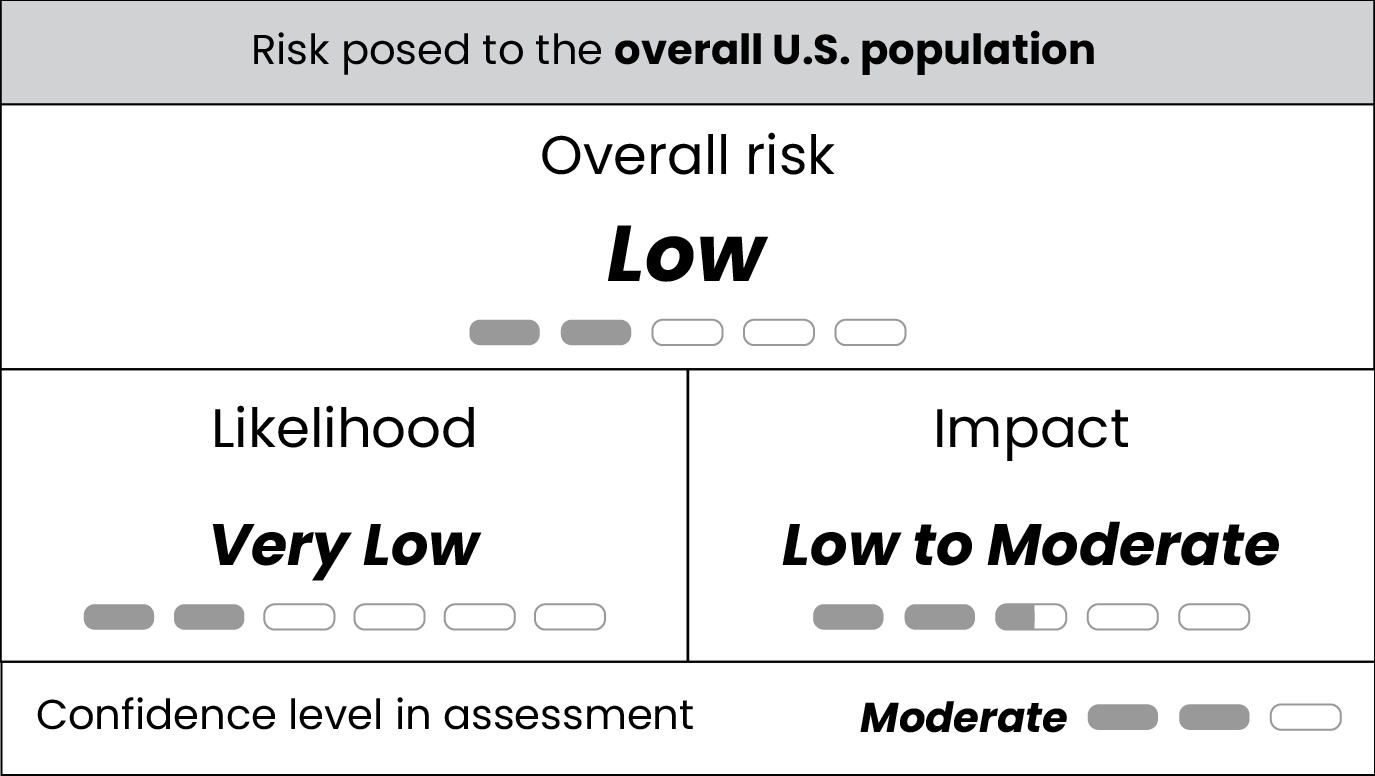
Risk to the overall U.S. population
Likelihood
If clade I mpox were to be introduced into the United States, we assess the likelihood of infection for the overall U.S. population would be very low.
If clade I mpox is introduced to the overall population in the United States, CDC experts believe transmission levels would likely be reduced compared to levels in DRC for several reasons, including smaller average household sizes, modeling results, increased access to improved sanitation and healthcare, and the lack of zoonotic reservoirs of disease. We address risk for specific populations in the sections below.
Impact
If clade I mpox were to be introduced into the United States, we assess the impact of infection for the overall U.S. population would be low to moderate.
Most of the United States population has no immunity to the virus that causes mpox, leading to potentially higher impacts of infection. Additionally, acquired immunity from previous infection with the virus that causes mpox is extremely low for the overall population. Vaccine-induced immunity from mpox vaccination during the 2022 clade II mpox outbreak is also very low across the overall population. During the 2022 clade II mpox outbreak, vaccination was targeted to those at highest risk of infection, including men who have sex with men (MSM) with certain risk factors and their partners. Furthermore, smallpox vaccination rates, which can offer some protection against mpox, declined substantially in the United States in the 1970s, when population-wide smallpox vaccination ceased due to eradication of the disease.
Of note, the reported case-fatality rate (CFR; 3%) in DRC from the ongoing clade I mpox outbreak is lower than reported rates from historical outbreaks (up to 11%). In addition to lower reported CFRs in the ongoing clade I mpox outbreak, morbidity and mortality from clade I mpox are likely to be lower in the United States as compared to DRC and neighboring countries in Central and Eastern Africa, because of greater access to high-quality supportive care and medical countermeasures, leading to potentially a lower impact of infection.
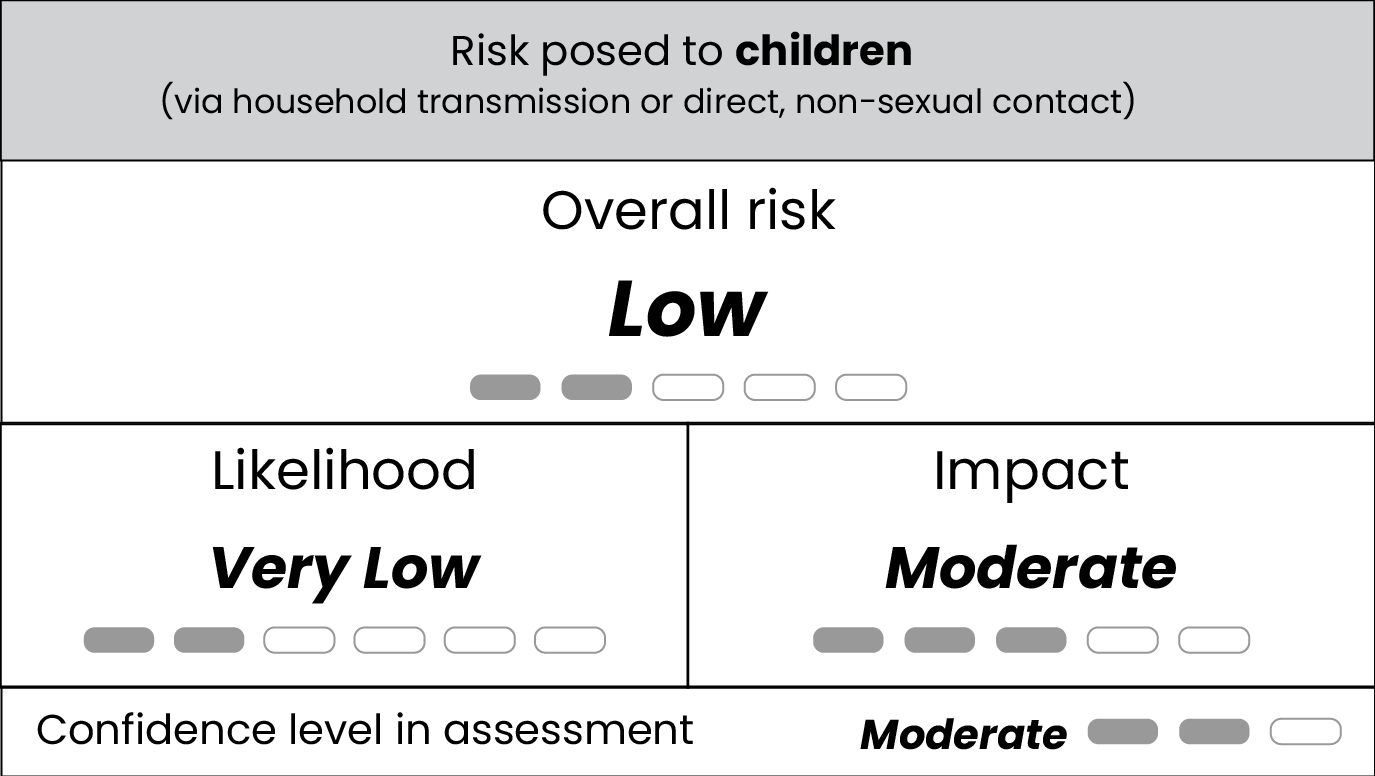
Risk to children
Likelihood
If clade I mpox were to be introduced to this population, we assess that the likelihood of infection for children for clade I mpox through household transmission and direct contact would be very low.
We do not expect transmission via household transmission or direct, non-sexual contact in the United States to reach levels observed in DRC, nor affect children to the same degree. Our assessment is based on modeling results, smaller proportion of children in the U.S. population (18% under 15 years of age in the United States compared to 46% in DRC), smaller average U.S. household size, generally increased access to improved sanitation and healthcare in the United States, and the lack of the virus that causes mpox circulating in animals in the United States.
CDC modeling suggests that direct contact transmission within and between households—including spread between children at daycares and schools—is unlikely to result in a large number of clade l mpox cases in the United States. Modeling results indicated that household transmission clusters would likely involve 10 or fewer mpox clade I cases, with minimal spread between households. Of note, these modeling results are based on clade Ia transmission dynamics and may be revised as new data become available on the more recently discovered clade Ib and its transmission dynamics.
We simulated household transmission through direct contact and transmission to other households through children's direct contact with other children at daycares and schools. Direct contact involves skin-to-skin contact and other direct contact with the virus that causes mpox, such as through sharing contaminated toys or bedding; this virus is not known to spread efficiently through respiratory secretions and is not known to be airborne.
Impact
If clade I mpox were to be introduced to this population, we assess that the impact posed to children for clade I mpox through household transmission and direct, non-sexual contact would be moderate.
In addition to the factors outlined in the above impact section, household and direct contact settings such as daycares or schools could be more impacted due to more significant disruption to daily activities and additional resources for public health measures. Mpox infection can be serious in children, and the vast majority of U.S. children have no immunity to mpox. Very few children in the United States have acquired immunity from either previous infection with the virus that causes mpox, or vaccination with mpox or smallpox vaccines.
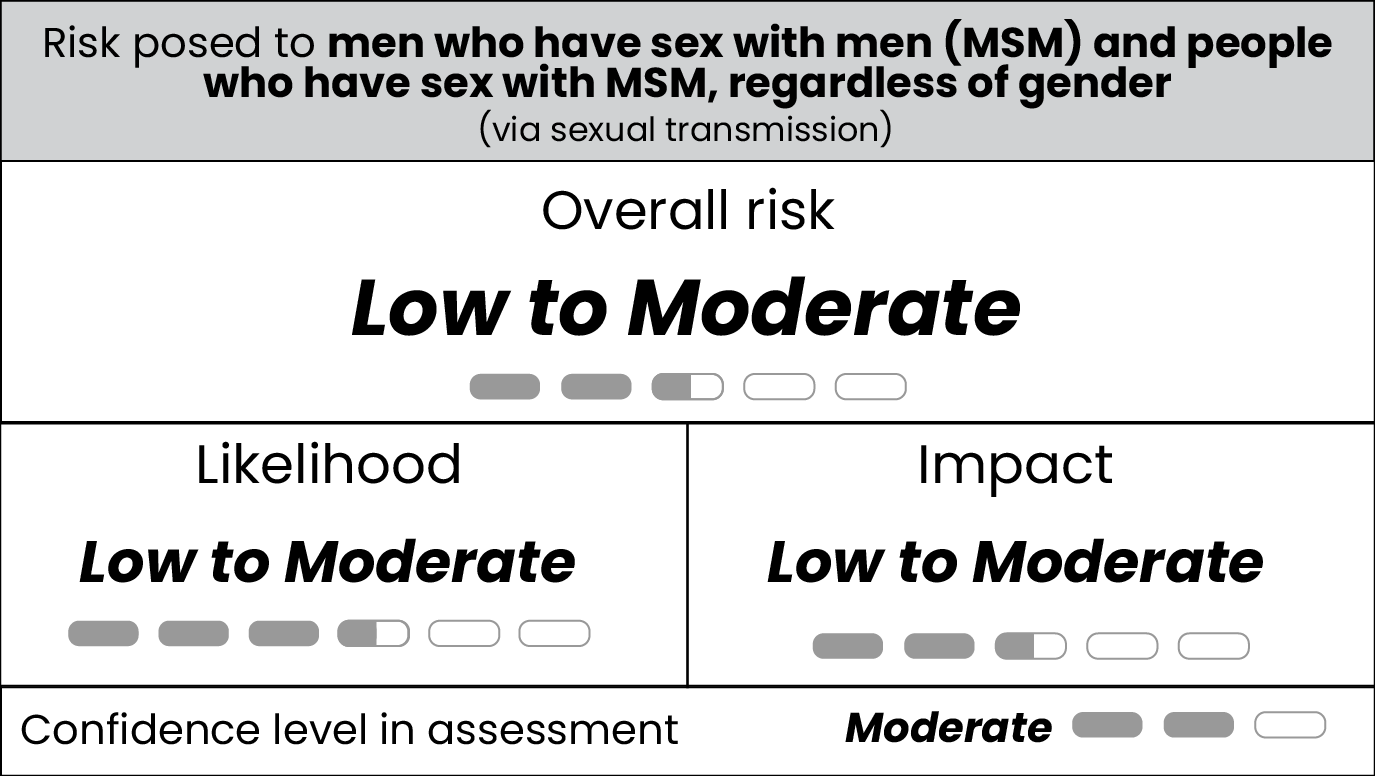
Risk to MSM via sexual transmission
Likelihood
If clade I mpox were to be introduced to this population, we assess the likelihood of infection via sexual transmission for MSM and for people who have sex with MSM, regardless of gender, is low to moderate. Of note, MSM with higher numbers of sexual partners may have a higher likelihood of exposure to the virus and thus their risk would be closer to the moderate risk range. If clade I mpox were introduced into this population, there would likely be sustained transmission of the virus, based on several factors, including widespread transmission in this population during the ongoing global clade IIb mpox outbreak that began in 2022, varying levels of population immunity, and insights from CDC modeling studies.
Most U.S. cases of clade IIb mpox were among MSM and their sexual partners, suggesting this population could have the highest likelihood of exposure for clade I mpox if the virus spread to U.S. sexual networks. Additionally, only a minority of MSM whom CDC has recommended would benefit from vaccination have been fully vaccinated, though rates vary widely by jurisdiction. However, population immunity to mpox infection might reduce the risk of infection with clade I mpox, depending on levels of vaccination uptake and mpox infection following the 2022 outbreak of clade IIb mpox, which varies across communities in the United States. In addition, during the 2022 global mpox outbreak in the United States, MSM reported behavior adaptations that likely contributed to declines in mpox incidence, indicating that similar changes could occur in future outbreaks, leading to a reduced likelihood of infection at a population level.
A 2023 modeling study estimated that a jurisdiction's risk for sustained mpox recurrence depends on population mpox immunity levels, finding some jurisdictions may have a high likelihood of sustained transmission. More recent CDC modeling found that counties with higher population-level immunity had decreased chances of a prolonged or large outbreak, relative to counties with lower immunity, if clade I mpox were to be introduced to MSM sexual networks in the United States. The study also found that counties with greater than 50% population-level immunity would have smaller outbreaks on average, involving fewer than 50 infections.
Impact
If clade I mpox were to be introduced to this population, we assess the impact of infection via sexual transmission for MSM and for people who have sex with MSM, regardless of gender, would be low to moderate.
In addition to the factors outlined in the above impact sections, population immunity among MSM and their sexual partners is likely to additionally reduce the severity of infection. However, population immunity varies greatly across communities in the United States, meaning some communities would have higher impacts of infection than others. Additionally, outbreaks concentrated in MSM communities, even if less severe than the 2022 clade IIb mpox outbreak, will have a large impact in these communities and require significant public health resources.
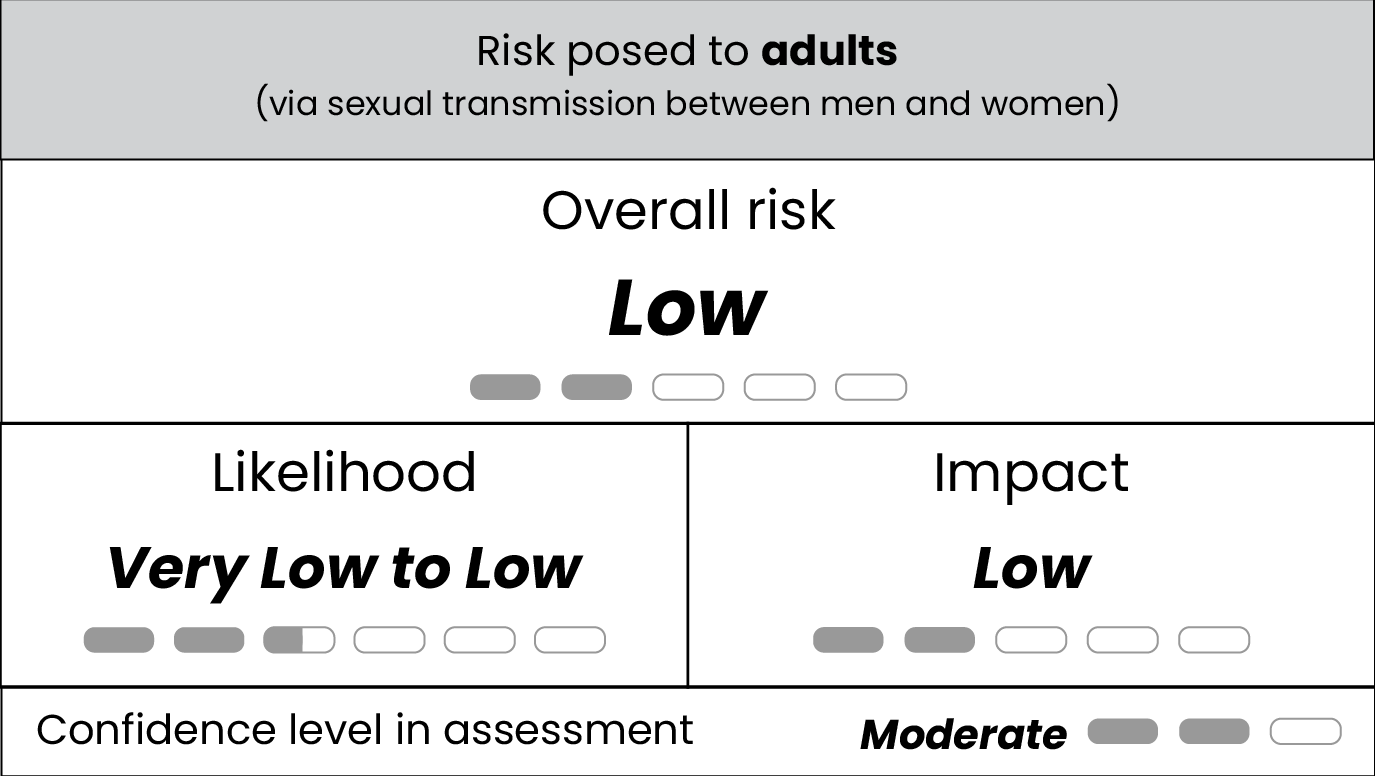
Risk to adults via sexual transmission between men and women
Likelihood
If clade I mpox were to be introduced into this population, we assess the likelihood of infection for adults via sexual transmission between men and women would be very low to low.
Sustained, widespread sexual transmission of clade I mpox in adults via sexual transmission between men and women in the United States is unlikely, based on lack of widespread transmission in heterosexual sexual networks during the 2022 global clade IIb mpox outbreak, as well as insights from modeling studies. A modeling study from the United Kingdom related to the 2022 outbreak indicated that lower partnership formation rates among heterosexuals prevented sustained transmission within these networks. Additionally, CDC modeling of the clade IIb outbreak has shown similar results for heterosexual sexual networks in the United States, indicating widespread transmission is unlikely.1 Results showed that clade I mpox could cause small clusters of cases in heterosexual sexual networks, including especially among sex workers and their contacts, and as such, likelihood of infection could be higher in these communities.
Evidence of sexual transmission and transboundary spread in Central and Eastern Africa could indicate an increased risk of spread if clade I mpox is introduced to the United States. Outbreaks of clade I mpox associated with female sex workers and their contacts have been reported in some DRC provinces. Recent genomic analyses suggest that transmission of clade Ib mpox is primarily human-to-human and not due to recurring zoonotic introductions. The role of different mpox subclades in changing transmission dynamics remains uncertain.
Impact
If clade I mpox were to be introduced to this population, we assess the impact of infection for adults via sexual transmission between men and women would be low.
In addition to the factors outlined in above impact sections, the impact of infection could be greater for sex workers and individuals in high-contact sexual networks. However, behavioral adaptation in affected populations could play a role in reducing transmission, similar to what CDC observed in the 2022 outbreak. That said, adaptation may be harder to achieve in the context of sex work due to its effect on people's livelihoods, and vaccination in this community may be a more effective method of prevention. CDC and other public health agencies will likely require additional public health resources to reach hard-to-reach populations like sex workers and their contacts, leading to a higher impact of infection in this community.
Confidence
We have moderate confidence in this assessment, increased from low confidence in our last assessment (released on August 30, 2024), as more data has been collected on both disease transmission and differences between clade subtypes in DRC and neighboring countries in Central and Eastern Africa. We note the following uncertainties:
- Implications for the United States are unclear due to the fact that most of the data from the recent spread of the clade I mpox outbreak originate in Central and Eastern Africa, which has different access to healthcare and social, economic, and cultural contexts.
- Limited epidemiologic and genomic data are available regarding outbreaks in Central and Eastern Africa, including lack of detailed transmission dynamics in children and sexual networks.
- Limited information is available on main routes of transmission and how these differ between the two circulating subclades of clade I Monkeypox virus, which leads to uncertainties in how extensively the virus could spread in the United States.
- Inadequate data on the levels of prior immunity in MSM and their sexual partners and the extent to which behavior adaptations initiated during the 2022 outbreak have continued or will return.
Factors that could change our assessment
- Further detection of clade I mpox cases in the United States, particularly if there is evidence of domestic person-to-person transmission
- Detection of clade I mpox outbreaks and sustained transmission in Europe or other regions with high volume of travel to the United States
- Extensive clade I mpox spread outside Central and Eastern Africa, including among people attending mass gatherings or among other highly mobile populations
- Further evidence of person-to-person spread in Central or East African countries, outside of already recognized activities that increase risk, such as exposure to animals or close contact with persons with mpox
- Further evidence of widespread, prolonged chains of sexual transmission in non-endemic countries
- Further evidence of differentiated epidemiological patterns between mpox clades Ia and Ib
- Data that suggests an increased or decreased illness severity of clade I mpox infection
- Increased mpox vaccination coverage among groups at increased risk in the United States
- Evidence of waning vaccine-induced immunity
Background and Methods
As of November 3, 2024, the DRC clade I mpox outbreak has resulted in more than 38,000 confirmed or suspected cases in 2024, including in Kinshasa and other urban areas of DRC. Cases in other regions of DRC with cross-border movement, such as Équateur and South Kivu Provinces, elevate the risk of disease spread outside of the country. As of November 3, 2024, there were 22 clade I mpox cases, including confirmed, probable, and suspected cases, in the neighboring Republic of the Congo, where clade Ia mpox is endemic. There are 67 confirmed clade I mpox cases in the neighboring Central African Republic, where clade Ia mpox is also endemic.
Clade lb mpox has more recently spread to non-endemic countries in Africa, including 1,509 confirmed cases in Burundi, 26 confirmed cases in Rwanda, 175 confirmed cases in Uganda, and 14 confirmed cases in Kenya, as of November 3, 2024. Epidemiologic data are limited for patients with mpox, and because of lack of laboratory confirmatory testing, we do not know the true number of cases. Sustained spread is occurring in Burundi and Uganda based on the geographic distribution of cases.
Since August 15, Sweden, Thailand, Germany, India, Zimbabwe, Zambia, and the UK have confirmed travel-associated cases of clade Ib mpox. These cases highlight the risk for travel-associated importations. If clade I mpox began to circulate person-to-person outside of the African continent, the potential for importation to the United States would increase.
Clade I mpox could potentially be introduced by infected travelers from DRC or other affected countries to the United States. Broader regional spread of clade I mpox in DRC and neighboring countries in Central and Eastern Africa increases the risk of importation to the United States. However, there are no direct commercial air passenger flights into the United States arriving from DRC, other countries where mpox is endemic, or where there are active outbreaks.
Monkeypox virus is divided into two clades (I and II) and four subclades (Ia, Ib, IIa, and IIb). Clade I has different transmission dynamics by subclade, with clade Ia spreading through multiple modes of transmission including contact with infected animals, household contact, and sexual contact. Clade Ib appears predominantly to be spread through intimate or sexual contact between adults.
Clade I mpox is endemic in Central Africa, and there are concurrent, ongoing outbreaks of clade I mpox in DRC. In previous outbreaks, clade I has caused a higher number of persons to have severe disease than clade II within close-contact settings, typically in a household. Historically, household transmission chains were typically small, although occasionally had involved up to six generations of transmission. While limited data are available, household transmission has likely played an important role in the current clade Ia outbreak in DRC, particularly for children. Transmission through patient care, in the absence of appropriate personal protective equipment, has also occurred. Transmission risk is highest among unvaccinated contacts; children and young adults are less likely to have vaccine-induced orthopoxvirus immunity since smallpox vaccination programs ended in DRC, other affected countries, and the United States.
Although clade I mpox is endemic in DRC, in 2023, health authorities began reporting a higher number of suspect cases and deaths across a wider geographic area that in some provinces affected atypical demographic groups. Approximately 66% of suspected mpox cases in DRC in 2024 were in children under age 15, similar to historical observations. However, areas that did not historically report mpox saw different transmission dynamics. For instance, adults were disproportionately affected in South Kivu province, where sexual transmission among adults was predominant. The South Kivu outbreak spread initially among female sex workers before becoming more broadly distributed, with one study finding more than 80% of hospitalized cases reporting recent sexual contact in bars. Sexual transmission of clade I mpox was also confirmed in a small outbreak affecting MSM and women in Kenge, Kwango Province, in March 2023.
The outbreaks in South Kivu and, more recently, in several East African countries, have been associated with clade Ib mpox. The younger age distribution of cases in Burundi—which has seen the most clade Ib cases outside of DRC—suggests that non-sexual transmission of clade Ib is also occurring. Clade Ib is a more recently detected sub-clade, and data from the DRC and a previous animal study suggests clade Ib mpox cases appear to be clinically milder than clade Ia mpox cases. In addition, clade Ib mpox cases in DRC and Burundi have been associated with a lower case fatality rate than clade Ia mpox cases.
As of October 23, 2024, CDC has not detected any cases of clade I mpox in the United States, despite testing a high proportion of presumed mpox specimens—those positive for non-variola orthopoxvirus (NVO)—with tests that can identify mpox by clade. In addition, several commercial and other non-CDC laboratories perform clade II testing in addition to NVO tests, and all specimens tested to date have been clade II. If these laboratories see anything unusual—for example, an NVO-positive but clade II-negative result—they are recommended to alert CDC immediately to ensure additional genotyping is conducted to determine if they are clade I. CDC continues to work, including with other U.S. government agencies, on multiple approaches to expand clade-specific testing domestically. Several public health laboratories have begun or are working to begin clade-specific testing.
CDC subject-matter experts specializing in risk assessment methods, infectious disease modeling, global health, and mpox and other orthopoxviruses collaborated to develop this rapid assessment. Experts initially convened in February 2024 to discuss the need for an assessment examining the risks posed by the DRC outbreak to the United States, key evidence related to the DRC outbreak, and specific populations to include in the assessment. To conduct this assessment, experts considered evidence including epidemiologic data from Central and Eastern Africa, data from the ongoing 2022 mpox outbreak in the United States caused by clade IIb, and historical data on clade I mpox outbreaks in DRC. After the initial assessment was finalized in February, experts subsequently re-reviewed evidence and updated this assessment in early March, mid-March, mid-April, late June, early August, and early October.
Overall risk was estimated by combining the likelihood of infection and the impact of the disease. For example, low likelihood of infection combined with high impact of disease would result in moderate risk. The likelihood of infection refers to the probability that members of the overall U.S. population acquire mpox—which in turn depends on the likelihood of exposure, infectiousness of the disease, and susceptibility of the population.The impact of infection considers several factors, including the severity of disease, level of population immunity, availability of treatments, and necessary public health response resources. A degree of confidence was assigned to each level of the assessment, taking into account evidence quality, extent, and corroboration of information.
For more details on our methods, please see our rapid risk assessment methods webpage.
Previous Updates
See our previous Mpox Risk Assessment since August 2024.
See other archived previous updates of the Mpox Rapid Risk Assessment.
- Pollock E, Nakazawa Y, Asher J, Gift T, Spicknall I. Potential mpox transmission among college-attending 18-25-year-olds with opposite-sex contacts in the United States. (2023, July 24-27). The International Society for Sexually Transmitted Diseases Research.
