What to know
The social determinants of health focus area includes tools and resources to inform and educate about "the non-medical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, development agendas, social norms, social policies, racism, climate change, and political systems."1

Introduction
This page is part of the Cervical Cancer Screening Change Package.
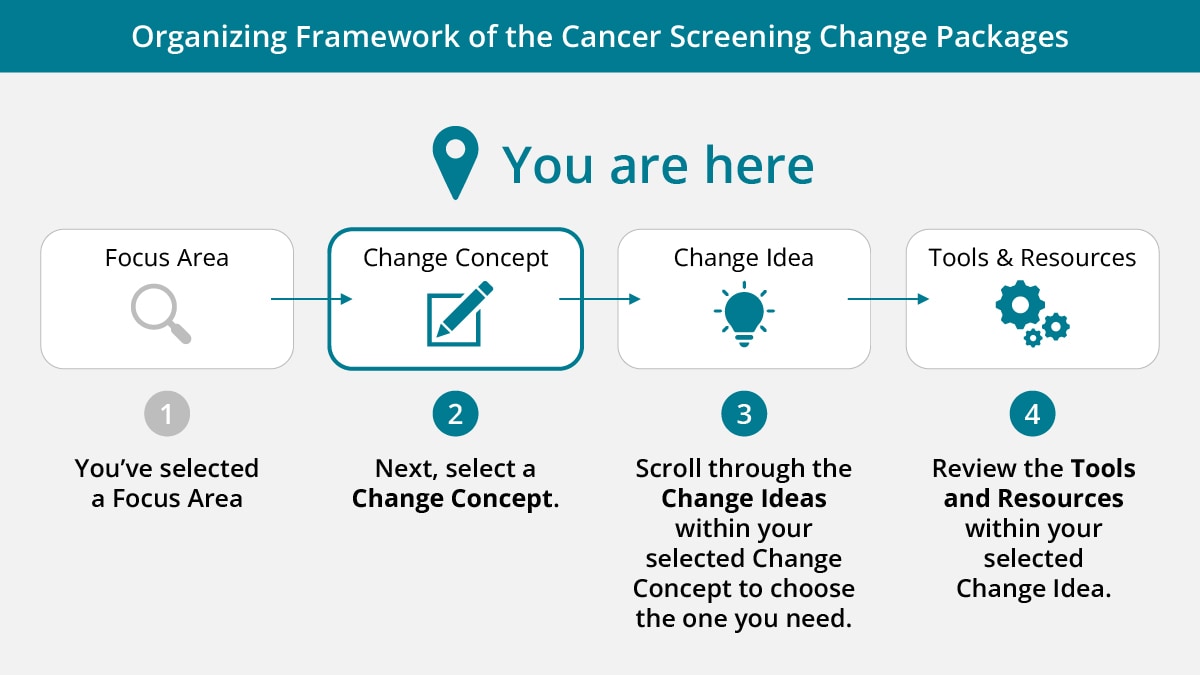
Change concepts are "general notions that are useful for developing more specific strategies for changing a process."2 Change ideas are evidence-based or practice-based "actionable, specific ideas or strategies."2 Each change idea is linked to tools and resources that can be used or adapted to improve cancer screening.
Note: See a list of acronyms used in this change package.
Select a change concept:
Change concept: Develop screening programs and jurisdictional cancer control plans and initiatives.
- CDC — The National Environmental Public Health Tracking Network
- CDC — PLACES: Local Data for Better Health
- CDC — CDC/ATSDR Social Vulnerability Index (SVI)
- CDC and HHS Office of Minority Health — Minority Health Social Vulnerability Index
- Census Bureau — Small Area Health Insurance Estimates (SAHIE) Program, see Health Insurance Interactive Data Tool
- HHS Office of Minority Health — Compendium of Federal Datasets Addressing Health Disparities
- NCI — Health Disparities Calculator (HD*Calc)
- U of M CARES (on Community Commons website) — Vulnerable Populations Footprint Tool
- UW PHI — County Health Rankings & Roadmaps
- Alcaraz KI, Wiedt TL, Daniels EC, Yabroff KR, Guerra CE, Wender RC, 2019 — Understanding and addressing social determinants to advance cancer health equity in the United States: A blueprint for practice, research, and policy [full text available]
- AMA — Organizational Strategic Plan to Embed Racial Justice and Advance Health Equity 2021–2023, see AMA Equity Strategic Plan (ama-assn.org), page 18
- Eslava-Schmalbach J, Garzón-Orjuela N, Elias V, Reveiz L, Tran N, Langlois EV, 2019 — Conceptual framework of equity-focused implementation research for health programs (EquIR) [full text available]
- Frieden TR, 2010 — A Framework for Public Health Action: The Health Impact Pyramid [full text available]
- King County, Washington — 2016–2022 Equity & Social Justice Strategic Plan: The "Unhealthy Stream" Creates Inequities and "Healthy Stream" Creates Equity [infographic]
- WHO — Closing the gap in a generation: health equity through action on the social determinants of health, see Commission on Social Determinants of Health conceptual framework, page 43
- Yearby R 2020 — Structural Racism and Health Disparities: Reconfiguring the Social Determinants of Health Framework to Include the Root Cause
- CDC — Program Evaluation
- CDC — National Breast and Cervical Cancer Early Detection Program: Writing Effective Objectives
- Eslava-Schmalbach J, Garzón-Orjuela N, Elias V, Reveiz L, Tran N, Langlois EV, 2019 — Conceptual framework of equity-focused implementation research for health programs (EquIR) [full text available]
- ACS and CCCNP — Cancer Plan Tip Sheets
- AICAF, UIHI, and NCUIH — American Indian Cancer Foundation Cancer Plan 2020–2022
- CDC — Comprehensive Cancer Control Programs
- CDC — Decision Matrix for Program 2 of Cancer Prevention and Control Programs for State, Territorial and Tribal Organizations funding opportunity DP22-2202: The National Comprehensive Cancer Control Program
- CDC — Networking 2Save
- CDC — United States Cancer Statistics (USCS): Data Visualizations Tool
- CMS — Disparities Impact Statement and Table of data sources to help identify health disparities and priority populations [these two resources are meant to be used together]
- CPCRN — Resources and Putting Public Health Evidence in Action
- President's Cancer Panel — Closing Gaps in Cancer Screening: Connecting People, Communities, and Systems to Improve Equity and Access
- RWJF — Understanding the Social Determinants of Health
- RWJF — Our Focus Areas
Change concept: Inform policies that can support cancer screening and treatment.
- Census Bureau — SAHIE
- President's Cancer Panel — Closing Gaps in Cancer Screening: Connecting People, Communities, and Systems to Improve Equity and Access
- CDC — Establishing Workplace Policies
- New York State Department of Health — Paid Leave: A Benefit for Employers and Employees
- Public Health and Tobacco Policy Center — Cancer Screenings: Workplace Policies to Improve Screening Rates, pages 6–7
- The Brookings Institution (Tomer A, Fishbane L, Siefer A, Callahan B, 2020) — Digital prosperity: how broadband can deliver health and equity to all communities
- CDC — Telehealth and Telemedicine: A Research Anthology of Law and Policy Resources
- FCC and NCI — FCC-NCI Broadband Cancer Collaboration
- Rural Health Information Hub (Mead A, 2021) — Broadband in Rural America: Faster Speeds for Home and Healthcare
Change concept: Inform about the availability of health insurance coverage.
- ACS — Cervical Cancer Prevention and Screening: Financial Issues [English and Spanish]
- ACS — Costs and Insurance Coverage for Cancer ScreeningA [English and Spanish]
- Volpara Health (Manning K, 2020) — The Medical Necessity Letter: Advocating to Get Your Patients the Care They Need
References
1Centers for Disease Control and Prevention. Social Determinants of Health at CDC. Accessed December 9, 2022.
2Centers for Disease Control and Prevention. Tobacco Cessation Change Package. US Department of Health and Human Services; 2019.
- Indicates a patient resource.
