Key points
- CDC conducts active surveillance for early-onset neonatal sepsis.
- Early-onset neonatal sepsis is a serious bloodstream infection in infants in the first days of life.
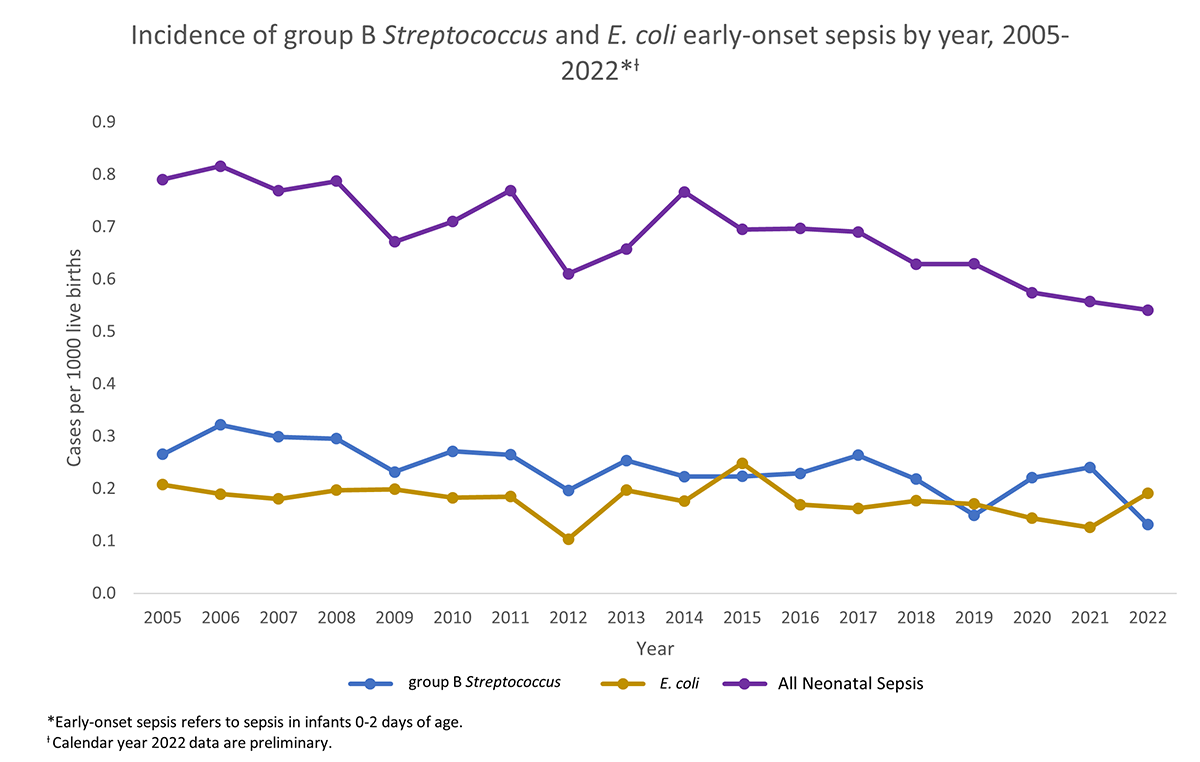
- Group B Streptococcus (GBS) and Escherichia coli (E. coli) bacteria are leading causes of early-onset neonatal sepsis.
- GBS early-onset neonatal sepsis has decreased due to GBS-associated primary prevention strategies.
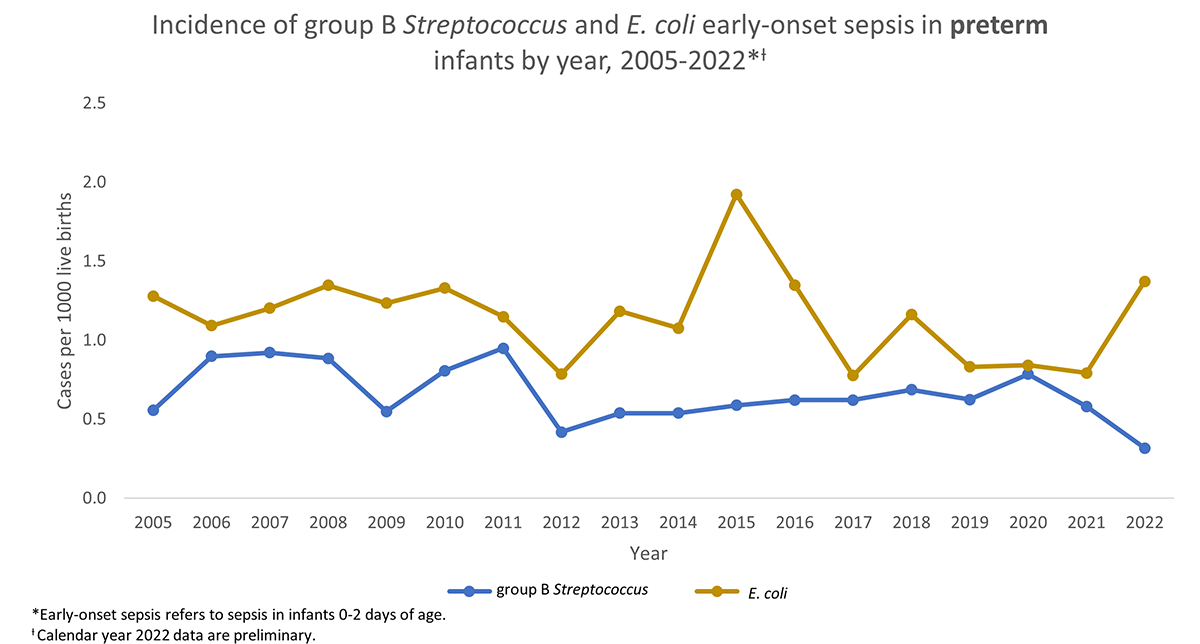
- The disproportionate burden of E. coli early-onset neonatal sepsis in preterm infants underscores the need for targeted prevention strategies.
Overview
Neonatal sepsis is a type of invasive disease that occurs when infants develop a bloodstream infection. Invasive disease refers to when bacteria invade parts of the body, like the blood, that are normally free from pathogens. Neonatal sepsis is associated with significant morbidity and mortality.
If sepsis develops in the first week of an infant's life, it's referred to as early-onset neonatal sepsis. Often researchers further limit this timeframe to the first 48 or 72 hours of life.
Tracking early-onset neonatal sepsis
Active Bacterial Core surveillance (ABCs) conducts active hospital- and laboratory-based surveillance for invasive bacterial pathogens of public health importance. In 2005, ABCs established surveillance for early-onset neonatal sepsis caused by bacterial infections in infants 0 through 2 days of age.
Surveillance population
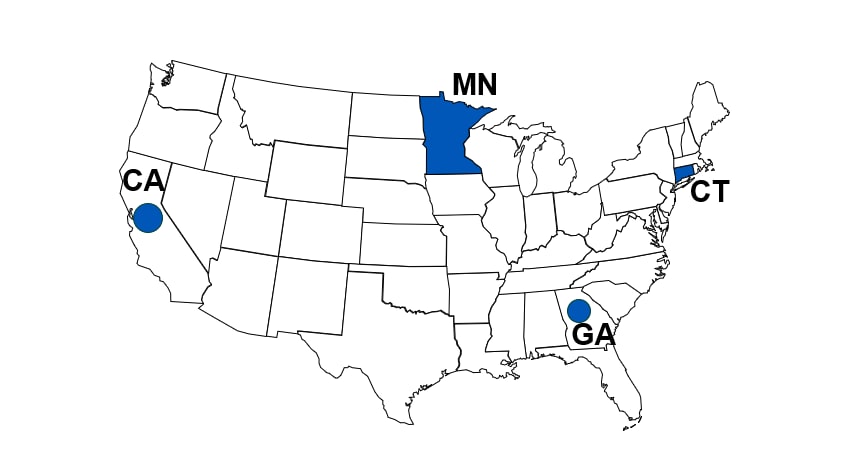
The following ABCs sites currently conduct surveillance for early-onset neonatal sepsis cases:
- California (CA): Select hospitals in 3 counties in the Bay area
- Connecticut (CT): Statewide
- Georgia (GA): Select hospitals in an 8-county metro area
- Minnesota (MN): Statewide
The surveillance area represents approximately 190,000 live births per year. ABCs calculates disease rates by pathogen and geographic area using the number of observed cases of neonatal sepsis as the numerator. ABCs uses the number of live births in the surveillance area hospitals as the denominator.
Surveillance sites
Case definition
ABCs includes cases if they meet all of the following criteria:
- Infant 0–2 days of age
- Bacterial pathogens isolated from blood or cerebrospinal fluid (CSF)
- Live birth of an infant at a hospital in the surveillance area
- Residence in the surveillance area isn't a requirement
- Residence in the surveillance area isn't a requirement
The specific bacterial pathogens include the ABCs and FoodNet pathogens.
ABCs excludes cases if any of the following are true:
- Infant ≤22 weeks gestation
- Infections caused by bacterial pathogens deemed contaminants
- Culture collected >12 hours after death
- Births outside of a surveillance area hospital (e.g., home birth)
- Stillbirths
Case ascertainment
ABCs identifies early-onset neonatal sepsis cases through
- Onsite cooperation of participating surveillance hospital personnel
- Audits of participating clinical laboratories
- Active reporting to the state surveillance system
Surveillance program staff complete standardized case report forms for each identified case. The forms include information on
- Demographic characteristics
- Clinical syndrome
- Illness outcome
- Pathogen antimicrobial susceptibility
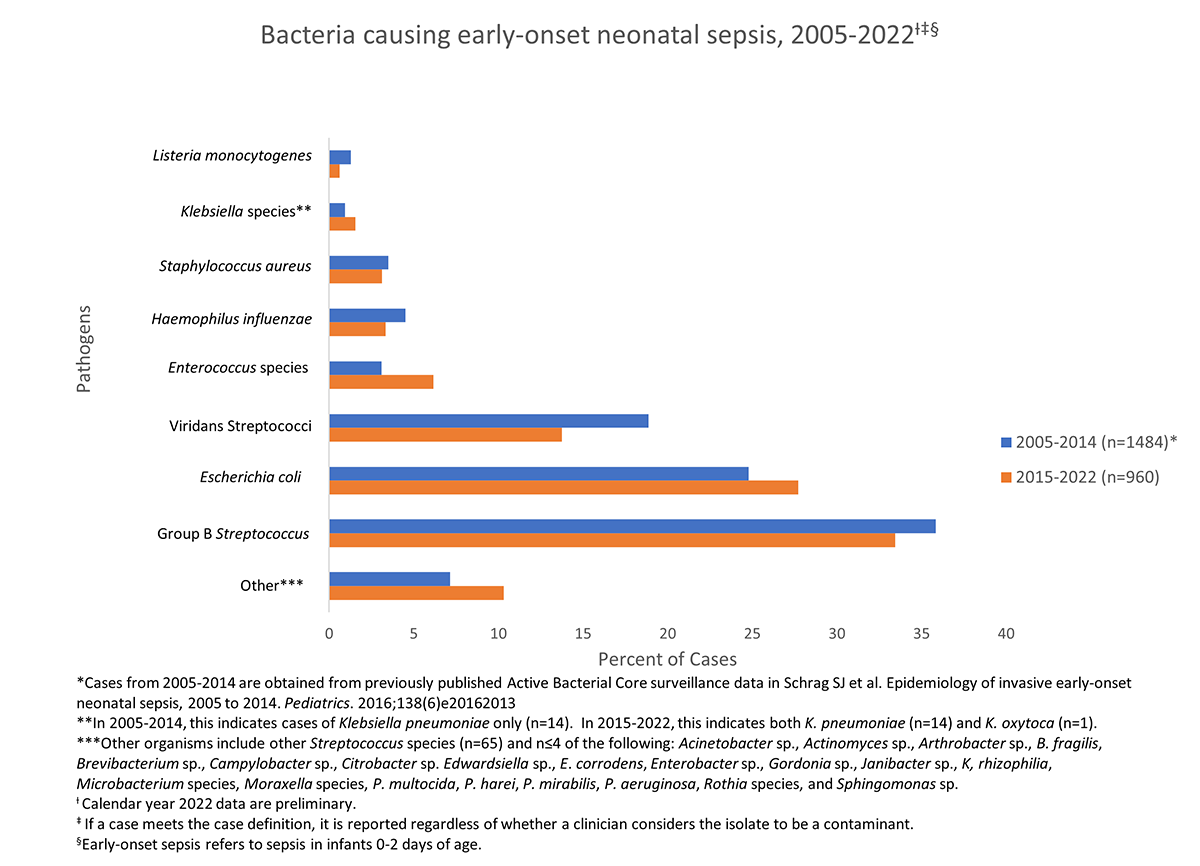
Most common bacterial causes
GBS and E. coli are leading causes of early-onset neonatal sepsis.
Overall incidence of GBS-associated early-onset neonatal sepsis has declined significantly since the introduction of primary prevention strategies in 1996. These strategies include the use of intrapartum antibiotic therapy for women identified to be at increased risk.
Continued surveillance is needed to further explore pathogen-specific strategies to reduce the early-onset neonatal sepsis burden even more.
Cause varies by gestational age and birthweight
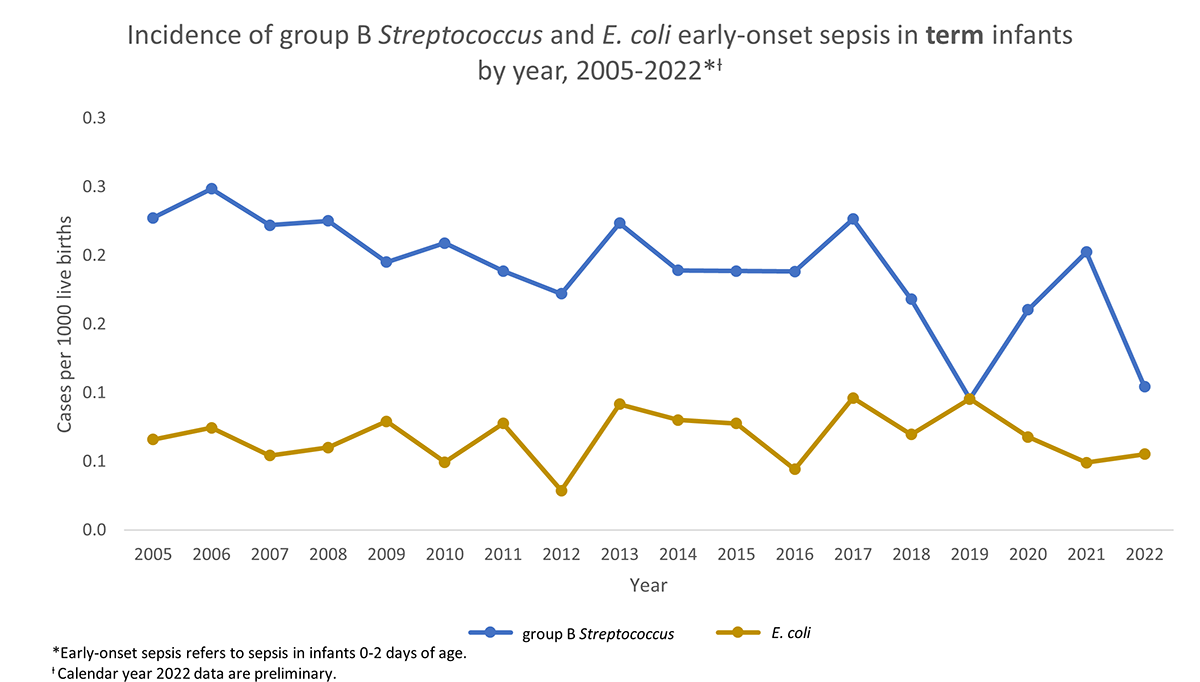
GBS is the most common cause of early-onset neonatal sepsis in term infants (born between 37 and 42 weeks of pregnancy). In comparison, E. coli is the most common cause in preterm infants (born before 37 weeks of pregnancy).
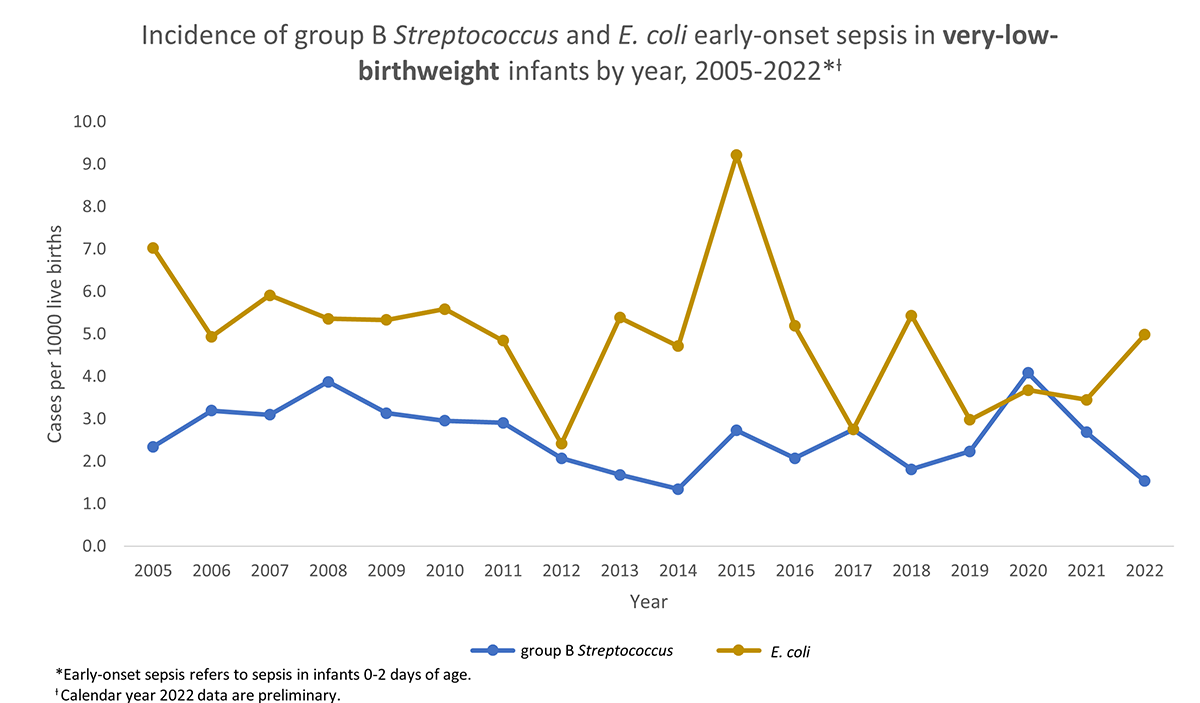
In very-low-birthweight infants who weigh less than 1500 grams at birth, E. coli is a more common cause.
The graphs below depict the incidence of GBS and E. coli early-onset neonatal sepsis in preterm, term, and very-low-birthweight infants.
Cause varies by gestational age
In preterm infants, the incidence of E. coli-associated early-onset sepsis is higher than GBS-associated early-onset sepsis in all surveillance years. In term infants, the incidence of GBS-associated early-onset sepsis is higher than E. coli-associated early-onset sepsis.
Cause in very-low-birthweight infants
During most surveillance years, incidence of E. coli early-onset sepsis is higher than GBS early-onset sepsis in very-low-birthweight infants.
Resource
Schrag SJ, Farley MM, Petit S, Reingold A, Weston EJ, Pondo T, Hudson Jain J, Lynfield R. Epidemiology of Invasive Early-Onset Neonatal Sepsis, 2005 to 2014. Pediatrics. 2016 Dec;138(6):e20162013.
