Key points
- Learn about the historic decreases CDC observed in the invasive bacterial disease burden caused by Active Bacterial Core surveillance (ABCs) pathogens.
- The COVID-19 pandemic and associated mitigation measures implemented early in the pandemic likely played a role in these decreases.
Overview
Each year ABCs releases data describing the burden and epidemiology of invasive disease due to
- Group A Streptococcus (GAS)
- Group B Streptococcus (GBS)
- Haemophilus influenzae (HFlu)
- Neisseria meningitidis
- Streptococcus pneumoniae (SPN)
ABCs released 2020 data with summary statistics comparing ABCs pathogen-specific incidence rates during the pandemic period to the pre-pandemic period. Neisseria meningitidis was not included in this commentary due to small numbers of reported cases. The pandemic period is defined as March to December 2020 and the pre-pandemic period is January 2014 to February 2020.
ABCs also included interpretations of how pandemic-related factors may have impacted ABCs pathogen disease burden.
View final ABCs data
Methods for estimating changes during the pandemic period
CDC defined the COVID-19 pandemic period of 2020 as March–December. This was based on widespread circulation of SARS-CoV-2 in the United States and implementation of non-pharmaceutical interventions. For example, social distancing resulting from remote work and school arrangements, and mask wearing.
CDC used interrupted time series analysis through Autoregressive Integrated Moving Average models fit to monthly incidence rates between January 2014–February 2020. This predicted pathogen-specific monthly incidence rates for March–December 2020. Predicted rates were compared to observed rates using incidence rate ratios (IRR) and 95% credible intervals (CIs) for the pandemic period. IRRs and CIs are reported as percentage change (1-IRR).
Key findings from 2020 ABCs surveillance data
In 2020, CDC observed historic decreases in the invasive bacterial disease burden caused by pathogens monitored by ABCs.
The COVID-19 pandemic and the associated mitigation measures implemented early in the pandemic likely played a role in these decreases.
| Changes in overall incidence of invasive bacterial infections during 10-month pandemic period (March–December 2020) ** | ||
|---|---|---|
| Pathogen | % | 95% credible interval |
| Group A Streptococcus | -28% | (-11% to -40%) |
| Group B Streptococcus | -12% | (-7% to -16%) |
| Haemophilus influenzae | -60% | (-50% to -67%) |
| Streptococcus pneumoniae | -58% | (-52% to -62%) |
**All ages
GAS findings
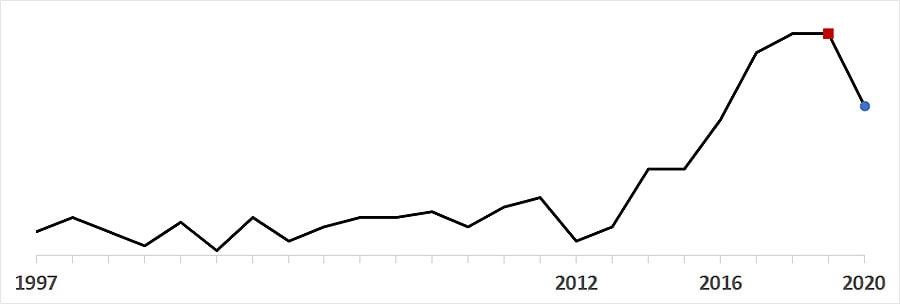
Annual incidence
Incidence of overall invasive GAS has increased each year since 2012. Overall invasive GAS incidence decreased from 7.6 cases per 100,000 population in 2019 (red square) to 6.1 in 2020 (blue circle). This was the lowest annual rate since 2016.
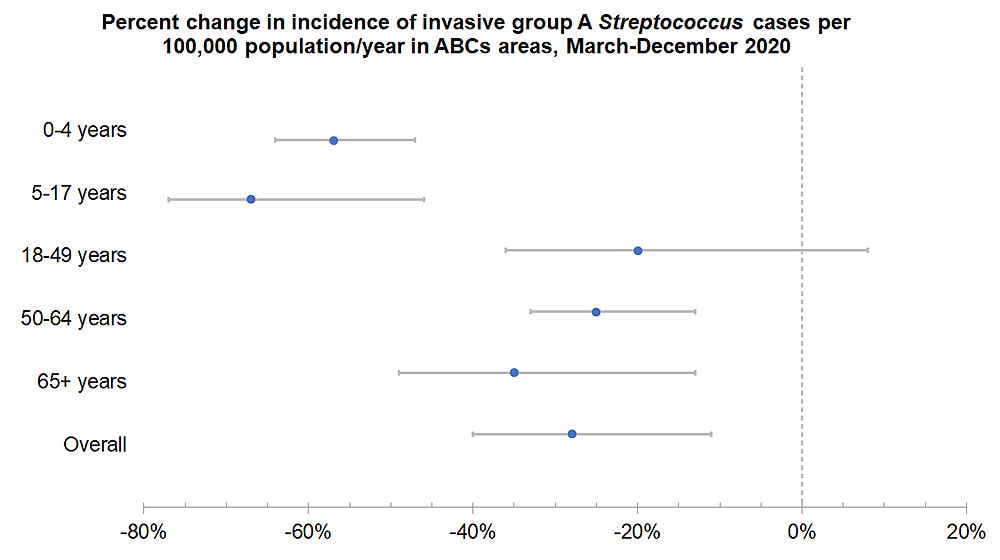
Declines by age group
Monthly invasive GAS rates were 28% lower than predicted during the pandemic period (IRR 0.72, 95% CI 0.60–0.89). The percentage change was greatest for children ages 5–17 years (65% lower than predicted, 95% CI 50–74%). Among adults, the greatest declines were in those aged ≥65 years (37% lower, 95% CI 12–51%).
GBS findings
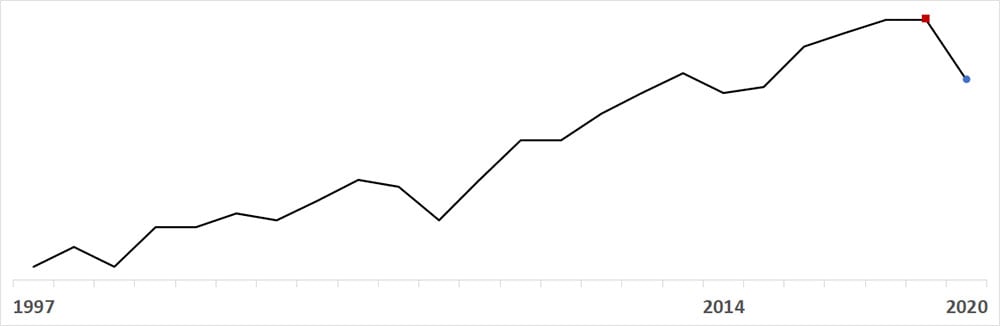
Annual incidence
Annual incidence of GBS has increased each year since 2014. Overall invasive GBS incidence decreased from 9.9 cases per 100,000 population in 2019 (red square) to 9.0 in 2020 (blue circle). This was the lowest annual rate since 2015.
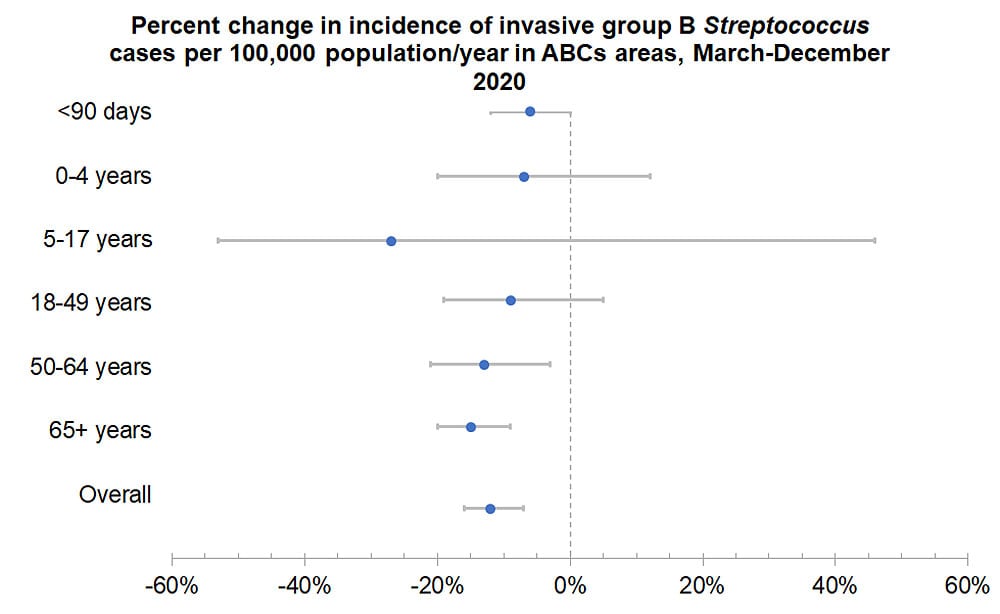
Declines by age group
Monthly invasive GBS rates were 12% lower than predicted during the pandemic period (IRR 0.88, 95% CI 0.84–0.93). No significant changes were observed for persons <50 years old, including invasive GBS disease among infants <90 days old.
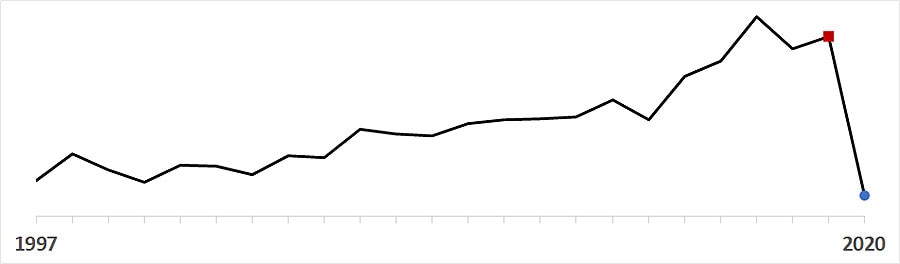
HFlu findings
Annual incidence
Overall invasive HFlu incidence dropped from 2.2 cases per 100,000 population in 2019 (red square) to 1.1 in 2020 (blue circle). This was the lowest annual incidence recorded since ABCs began in 1997.
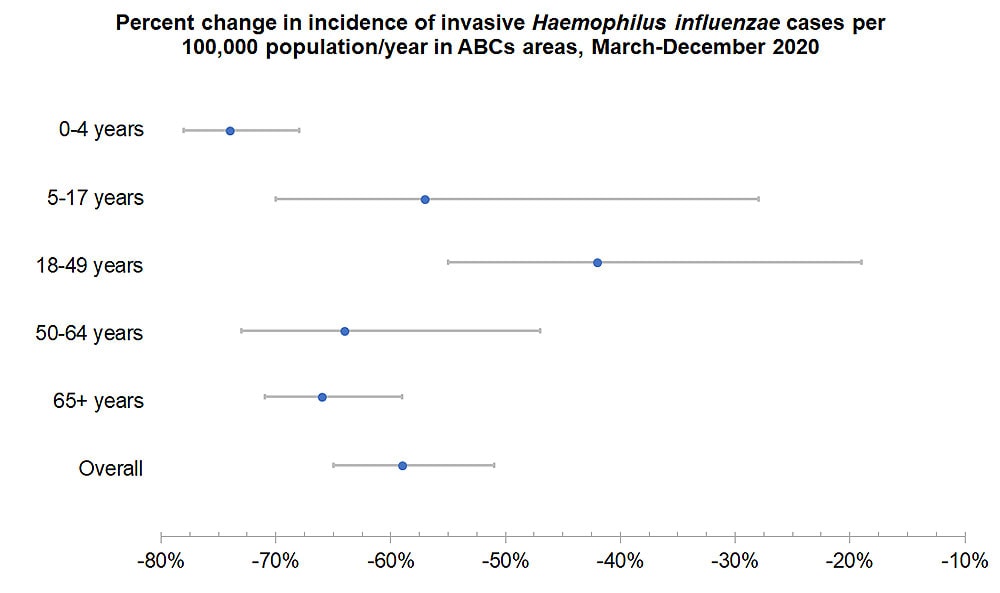
Declines by age
Monthly invasive HFlu rates were 60% lower than predicted during the pandemic period (IRR 0.40, 95% CI 0.33–0.50). The percentage change was greatest for children aged 0–4 years (76% lower, 95% CI 70–80%).
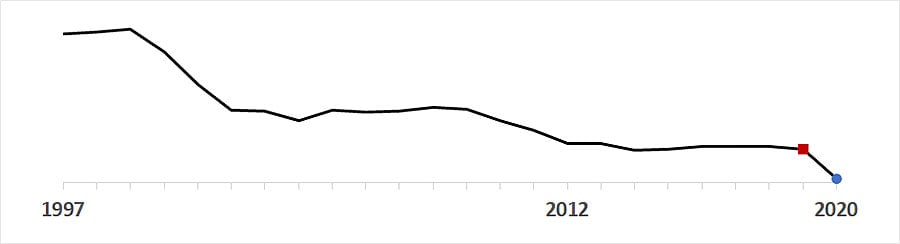
SPN findings
Annual incidence
SPN annual incidence fluctuated between 9.1 and 9.9 from 2012 through 2018. Overall invasive SPN incidence dropped from 9.2 cases per 100,000 population in 2019 (red square) to 5.4 in 2020 (blue circle).
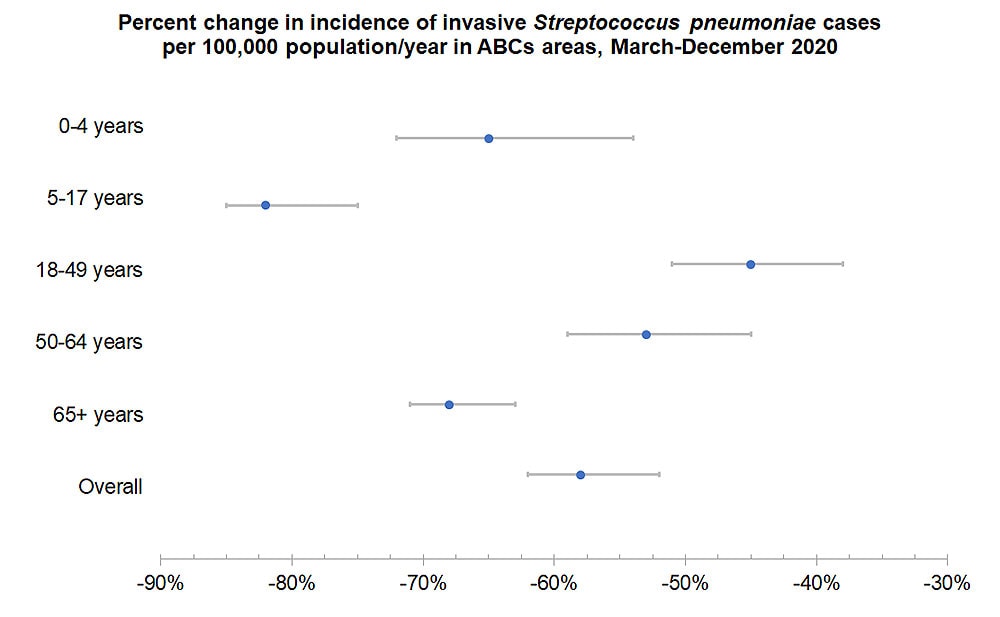
Declines by age
Monthly SPN rates were 58% lower than predicted during the pandemic period (IRR 0.42, 95% CI 0.38–0.48). The percentage change was greatest for children ages 5–17 years (83% lower than predicted, 95% CI 77–86%). Among adults, the greatest declines were in those aged ≥65 years (68% lower, 95% CI 63–71%).
Interpreting 2020 changes
Compared to previous years
2020 noted the largest single-year decreases in the of incidence disease caused by of GAS, GBS, HFlu, and SPN with one exception. There was a large drop in SPN in 2001. This was associated with the introduction of pneumococcal conjugate vaccine (PCV7) among children <5 years old in 2000.
No change in methods
The reported 2020 infections reflect true decreases in invasive bacterial disease identified by laboratory-based isolation from a normally sterile site. They are not due to changes in surveillance methods. On-going assessment of case ascertainment indicators confirmed that case capture remained high and comparable to previous years.
Impact of COVID-19 pandemic
COVID-19-associated non-pharmaceutical interventions likely reduced invasive bacterial disease due to bacteria typically transmitted via respiratory droplets. This includes GAS, HFlu, and SPN, as well as those transmitted via direct contact, such as GBS.
Widespread interventions to limit the spread of SARS-CoV-2, the virus that causes COVID-19, likely contributed to fewer exposures to ABCs pathogens. Interventions went into effect in March 2020 and drastically reduced in-person interactions. These include school and workplace closures, cancellation of public events, and gathering restrictions.
The pandemic and corresponding public health response make explaining changes in the observed incidences of invasive bacterial infections challenging. In addition to factors mentioned here, unknown factors might have contributed to fewer exposures, infections, and detections. Continued surveillance and laboratory characterization of ABCs pathogens may improve CDC’s understanding of how the pandemic affected the incidence of infections. It may also identify new prevention strategies.
