At a glance
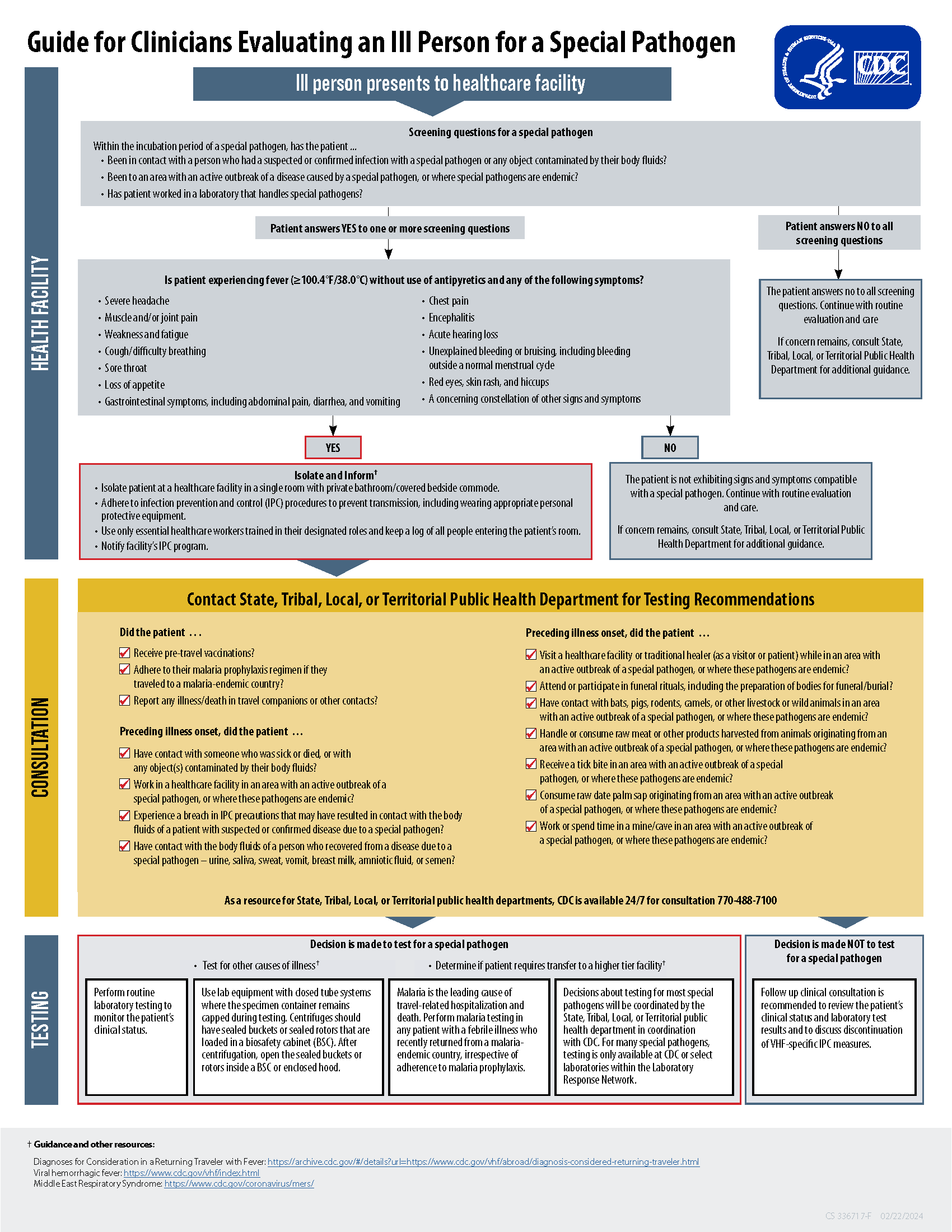
Healthcare providers should conduct an initial screening to determine if a patient has relevant exposure history and clinical signs consistent with a viral hemorrhagic fever (VHF) or high-consequence disease. After an initial screening, if a healthcare provider suspects a patient may have a VHF or other high-consequence disease, they should immediately follow the infection prevention guidance below and contact their health department for testing recommendations.

Scope of guidance
This guidance applies to VHFs caused by infections with:
- Filoviruses (ebolaviruses and marburgviruses),
- Arenaviruses [Lassa, Lujo, and South American hemorrhagic fever viruses (Guanarito virus, Sabia virus, Junin virus, Chapare virus, Machupo virus)],
- Rift Valley fever virus, and
- Crimean-Congo hemorrhagic virus.
This guidance applies to other high-consequence diseases caused by viruses that require a specialized laboratory, are highly pathogenic, and have no vaccine or treatment currently available, like Nipah virus.
Initial screening questions
To screen an ill person presenting to a healthcare facility for a suspect viral hemorrhagic fever (VHF) or other high-consequence disease, ask the patient if they have:
- Been in contact with a person who had a suspected or confirmed infection with a VHF or other high-consequence disease or any object contaminated by their body fluids?
- Been to an area with an active outbreak of a disease caused by a VHF or other high-consequence disease, or where these diseases are endemic?
- Worked in a laboratory that handles VHFs or other high-consequence disease?
If the patient answers "No" to all screening questions, continue with routine evaluation and care. If concern remains, consult your health department for additional guidance.
If the patient answers "Yes" to one or more screening questions, ask about signs or symptoms compatible with a VHF or other high-consequence disease. Is the patient experiencing fever (100.4°F/38.0°C) without use of antipyretics and any of the following symptoms?
- Severe headache
- Muscle and/or joint pain
- Weakness and fatigue
- Cough/difficulty breathing
- Sore throat
- Loss of appetite
- Gastrointestinal symptoms, including abdominal pain, diarrhea, and vomiting
- Chest pain
- Encephalitis
- Acute hearing loss
- Unexplained bleeding or bruising, including bleeding outside a normal menstrual cycle
- Red eyes, skin rash, and hiccups
- A concerning constellation of other signs and symptoms
If the patient is not reporting signs and symptoms compatible with a VHF or other high-consequence disease, continue with routine evaluation and care. If concern remains, consult your health department for additional guidance.
If the patient answered "Yes" to one or more screening questions AND is experiencing symptoms compatible with a VHF or other high-consequence disease, follow these recommended infection prevention and control (IPC) precautions for preventing transmission:
- Isolate the patient at a healthcare facility in a single room with private bathroom/covered bedside commode.
- Adhere to IPC procedures to prevent transmission, including wearing appropriate personal protective equipment (PPE).
- Use only essential healthcare workers trained in their designated roles and keep a log of all people entering the patient's room.
- Notify the facility's IPC program.
Contact health department
Once the patient is safely isolated, consult your state, tribal, local, or territorial public health department for testing recommendations. During this consultation, an in-depth public health interview will be conducted to review detailed travel and epidemiologic history and clinical course of the patient.
Conduct public health interview
Your health department will assist in conducting a thorough public health interview. Questions related to risk exposure, like those below, can help inform testing recommendations.
Did the patient:
- Receive pre-travel vaccinations?
- Adhere to their malaria prophylaxis regimen if they traveled to a malaria-endemic country?
- Report any illness/death in travel companions or other contacts?
- Have contact with someone who was sick or died, or with any object(s) contaminated by their body fluids?
- Work in a healthcare facility in an area with an active outbreak of a VHF or other high-consequence disease, or where these diseases are endemic?
- Experience a breach in IPC precautions that may have resulted in contact with the body fluids of a patient with a suspected or confirmed VHF or other high-consequence disease?
- Have contact with the body fluids of a person who recovered from a VHF or other high-consequence disease – urine, saliva, sweat, feces, vomit, breast milk, amniotic fluid, or semen?
- Visit a healthcare facility or traditional healer (as a visitor or patient) while in an area with an active outbreak of a VHF or other high-consequence disease, or where these diseases are endemic?
- Have contact with bats, pigs, rodents, camels, or other livestock or wild animals in an area with an active outbreak of a VHF or other high-consequence disease, or where these diseases are endemic?
- Handle or consume raw meat or other products harvested from animals originating from an area with an active outbreak of a VHF or other high-consequence disease, or where these diseases are endemic?
- Receive a tick bite in an area with an active CCHF outbreak, or where CCHF is endemic?
- Consume raw date palm sap originating from an area with an active Nipah outbreak, or where Nipah is endemic?
- Work or spend time in a mine/cave in an area with an active orthoebolavirus and orthomarburgvirus outbreak, or where these pathogens are endemic?
Make testing decisions in consultation with health department
If not testing for a VHF or other high-consequence disease
- Follow-up clinical consultation is recommended to review the patient's clinical status and laboratory test results
- Discuss discontinuation of VHF/ high-consequence disease-specific IPC measures.
If testing for a VHF or other high-consequence disease:
- Also test for other causes of illness and determine if the patient requires transfer to a higher-tier facility.
- Perform routine laboratory testing to monitor the patient's clinical status.
- Use lab equipment with closed tube systems where the specimen container remains capped during testing. Centrifuges should have sealed buckets or sealed rotors that are loaded in a biosafety cabinet (BSC). After centrifugation, open the sealed buckets or rotors inside a BSC or enclosed hood.
- Malaria is the leading cause of travel-related hospitalizations and deaths. Perform malaria testing in any patient with a febrile illness who recently returned from a malaria-endemic country, irrespective of adherence to malaria prophylaxis.
- Decisions about testing for most VHFs or other high-consequence diseases will be coordinated by the state, tribal, local, or territorial public health department in coordination with CDC. Testing for these diseases may only be available at CDC or select laboratories within the Laboratory Response Network.