Key points
This chapter provides general guidance for vaccine-preventable disease surveillance, describing the disease background/epidemiology, case investigation and reporting/notification, disease case definitions, and activities for enhancing surveillance, case investigation, and outbreak control for poliomyelitis.
Disease Description
Poliomyelitis is a highly contagious disease caused by 3 serotypes of poliovirus. Infection with poliovirus results in a spectrum of clinical manifestations from inapparent infection to nonspecific febrile illness, aseptic meningitis, paralytic disease, and death. Two phases of acute symptomatic poliovirus infection can be distinguished: a nonspecific febrile illness (minor illness) followed, in a small proportion of patients, by aseptic meningitis and/or paralytic disease (major illness). The ratio of cases of paralytic disease to mild/inapparent infection among susceptible individuals ranges from 1:200 to 1:1900. Following poliovirus exposure, viral replication occurs in the oropharynx and the intestinal tract. Viremia follows, which may result in infection of central nervous system cells. The virus attaches and enters cells via a specific poliovirus receptor. Replication of poliovirus in motor neurons of the anterior horn and brain stem results in cell destruction and causes the typical clinical manifestations of poliomyelitis. Depending on the site of neurocellular infection and subsequent paralysis, poliomyelitis can be classified as a spinal, bulbar, or spino-bulbar disease. Progression to maximum paralysis is rapid (2–4 days); paralysis is usually associated with fever and muscle pain, and rarely progresses after the temperature has returned to normal. Spinal paralysis is typically asymmetric, more severe proximally than distally, and deep tendon reflexes are absent or diminished. Bulbar paralysis may compromise respiration and swallowing. Historically, between 2% and 10% of paralytic poliomyelitis cases have been fatal. Following the acute paralytic episode, many patients recover muscle functions at least partially, and a prognosis for recovery can usually be established within six months after onset of paralytic manifestations. Starting about 15–40 years after the initial infection, about 25–40% of paralytic polio survivors will develop post-polio syndrome (PPS). This condition is manifest by muscle weakness in the affected limb(s), mental and physical fatigue, and joint pain. PPS is rarely life-threatening but can make it difficult for those affected to function independently. Infection with poliovirus is assumed to result in lifelong, type-specific immunity.
Background
Poliomyelitis became an epidemic disease in the United States at the turn of the 20th century. Epidemics of ever-increasing magnitude occurred as the decades progressed, with more than 20,000 cases of poliomyelitis with permanent paralysis reported in 1952. Following the introduction of effective vaccines— inactivated poliovirus vaccine (IPV) initially in 1955, then oral poliovirus vaccine (OPV) starting in 1961—the reported number of poliomyelitis cases in the United States declined dramatically to <100 cases in 1965 and to <10 cases in 1973. Additionally, with the introduction and widespread use of OPV (containing live attenuated poliovirus strains), vaccine-associated paralytic poliomyelitis (VAPP) was recognized. The risk of VAPP is highest following the first dose of OPV and among immunodeficient persons. VAPP was very rare, with an average of eight reported cases annually during 1980–1999, or one case reported for every 2.4 million doses of OPV distributed.12 By 1973, for the first time in the United States, more cases of VAPP were reported than paralytic disease caused by wild poliovirus.3 As this trend continued, in 1997 the Advisory Committee on Immunization Practices (ACIP) recommended changing to a sequential polio immunization schedule that included two doses of IPV, followed by two doses of OPV.4 VAPP occurred less frequently under this schedule, and in 2000, this recommendation was updated to a schedule of all IPV.567 OPV is no longer manufactured or available in the United States.
Figure 1: Total number of reported paralytic poliomyelitis cases—United States, 1980–2022
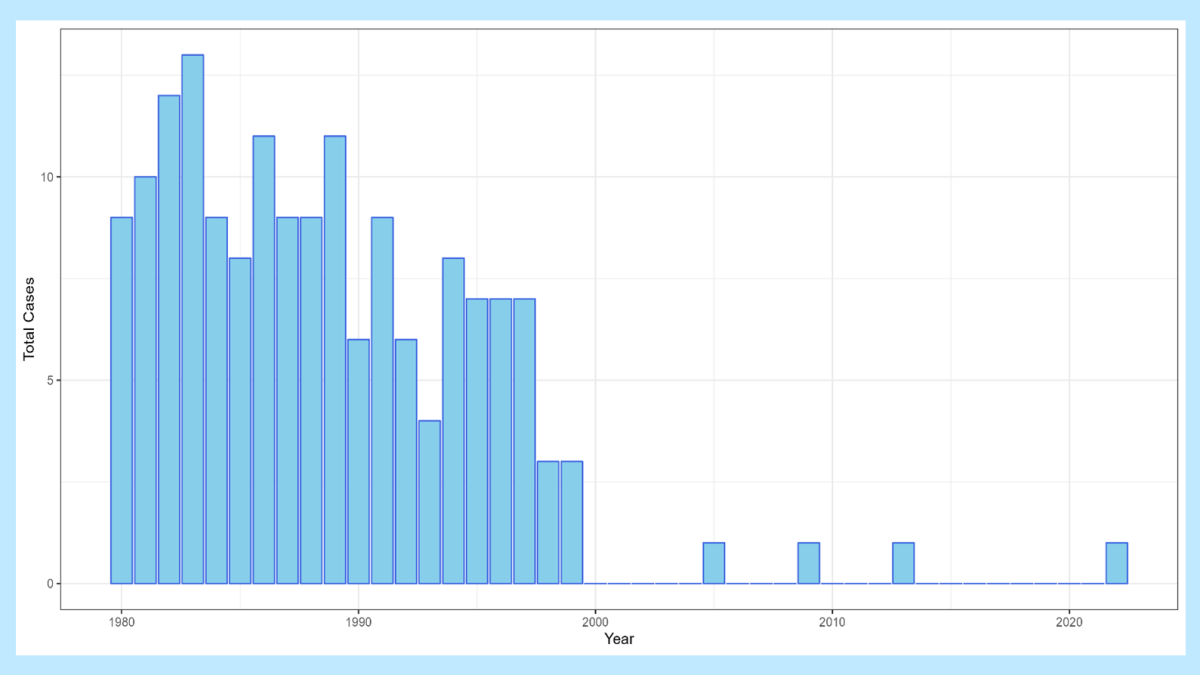
In the United States, the last cases of indigenously transmitted wild poliovirus disease were reported in 1979, and the last imported case of poliomyelitis caused by wild type poliovirus was reported in 199312 (see Figure 1). Since changing to an all-IPV immunization schedule in 2000, there have been only three cases of VAPP reported in the United States: one imported case, one in an immunocompromised person who was most likely exposed to OPV before its use was discontinued, and one fatal case in an immunocompromised child who was given OPV as part of routine childhood immunizations in India.8910
In 1988, the World Health Assembly adopted the goal of worldwide eradication of poliomyelitis by the year 2000.11 By 2001, substantial progress toward global eradication had been reported: a >99% decrease in the number of reported cases of poliomyelitis was achieved.12 Wild poliovirus type 2 was declared eradicated in 2015, followed by wild poliovirus type 3 in 2019.13 As of 2023, wild poliovirus type 1 (WPV1) remains endemic in just two countries: Afghanistan and Pakistan. However, importations of WPV1 into southern Africa (Malawi and Mozambique) were detected in 2022.14
The emergence of a circulating vaccine-derived poliovirus (cVDPV) causing an outbreak of poliomyelitis was first reported in Hispaniola in 2000.15 Since that initial outbreak, one or more cVDPV outbreaks have been reported each year.16 These outbreaks have generally occurred in regions where OPV is used and overall routine polio vaccination rates are low. cVDPVs are able to replicate in the intestinal tract of inadequately immunized persons and may be transmitted to others with inadequate immunity. During sustained transmission, the viruses may regain some of the properties of wild polioviruses, such as transmissibility and neurovirulence. Clinical disease caused by cVDPVs is indistinguishable from that caused by wild polioviruses. A majority of cVDPV outbreaks were caused by cVDPV type 2 (cVDPV2). To remove the risk for infection with cVDPV2, all OPV-using countries simultaneously switched in April 2016 from trivalent OPV (tOPV) to bivalent OPV (bOPV), which contains only types 1 and 3 polioviruses.17 However, despite this change, the number of cVDPV2 outbreaks increased after the switch, and >22 countries have experienced paralytic cases as a result of a cVDPV2. Monovalent OPV2 vaccine has been used to stop these outbreaks, but a drawback of using this vaccine is that it can circulate in undervaccinated communities to seed new cVDPV2 outbreaks. More recently, a novel OPV2 vaccine (nOPV2) was created that has decreased ability to revert to a neurovirulent virus.18 Find more information on the status of poliomyelitis eradication.
The potential for importation of wild poliovirus and cVDPV into the United States remains until worldwide poliomyelitis eradication is achieved. Universal vaccination of infants and children is critical for prevention of poliomyelitis cases and epidemics caused by importation of poliovirus into the United States. Population-based surveys conducted during 2009–2010 and 2012–2013 confirmed that the prevalence of poliovirus antibodies among school-age children, adolescents, and young adults in the United States was high (>90% to poliovirus types 1 and 2, and >83% to type 3).1920 Seroprevalence surveys conducted in two inner-city areas of the United States (areas in which routine coverage was low) during 1990–1991 also found that >80% of all children 12–47 months of age had antibodies to all three poliovirus serotypes.21 National coverage for three doses of IPV by age 24 months was 93.4% among infants born during 2018–2019.22 However, members of certain groups with low vaccination coverage remain susceptible to poliomyelitis.
In July 2022, the New York State Department of Health (NYSDOH) notified CDC of detection of poliovirus type 2 in stool specimens from an unvaccinated immunocompetent young adult from Rockland County, New York, who was experiencing acute flaccid weakness. Vaccine-derived poliovirus type 2 (VDPV2) was detected in stool specimens from the patient, and in wastewater samples from the patient's county of residence and in neighboring counties both before and after the patient's symptom onset. This is the second identification of community transmission of poliovirus in the United States since 1979. As of November 2023, no additional paralytic cases have been detected, and the last detection of poliovirus in wastewater occurred in February 2023. The occurrence of this case, combined with the identification in wastewater in multiple counties, underscores the importance of maintaining high vaccination coverage to prevent paralytic polio in persons of all ages.23
Importance of Rapid Identification
Rapid investigation of suspected poliomyelitis cases is critical for identifying possible poliovirus transmission. Rapid detection of cases permits the timely implementation of public health measures (e.g., vaccination) to limit the spread of imported wild poliovirus or cVDPVs to maintain elimination of poliomyelitis caused by poliovirus in the United States. Moreover, rapid investigation of suspected cases will allow collection of specimens for poliovirus confirmation, which is critical for determining whether a case of paralytic poliomyelitis is the result of wild or vaccine-derived virus infection.
Importance of Surveillance
The poliomyelitis surveillance system serves to detect cases of paralytic polio caused by wild or vaccine-derived polioviruses into the United States.
Disease Reduction Goals
No cases of paralytic polio due to indigenously acquired wild poliovirus have been reported in the United States since 1979, but in 2022 a case of paralysis due to a cVDPV2 was detected. There have been three reported cases of VAPP in the United States since 2000, when the use of OPV was discontinued. High coverage with poliovirus vaccine is required to maintain elimination of poliomyelitis in the United States until global eradication is achieved.
Case Definition
The following case definition for paralytic poliomyelitis and nonparalytic poliovirus infection has been approved by the Council of State and Territorial Epidemiologists (CSTE) and was published in 2023.24
Clinical Criteria:
Acute onset of flaccid paralysis with decreased or absent tendon reflexes in the affected limbs, in the absence of a more likely alternative diagnosis.
Laboratory Criteria
Confirmatory Laboratory Evidence:
- poliovirus detected by sequencing of the capsid region of the genome by the CDC Poliovirus Laboratory,
OR
- poliovirus identified in an appropriate clinical specimen (e.g., stool [preferred], cerebrospinal fluid, oropharyngeal secretions) using a properly validated assay,
AND
- specimen is not available for sequencing by the CDC Poliovirus Laboratory.
Case Classifications:
Confirmed:
Paralytic Poliomyelitis: Meets clinical criteria AND confirmatory laboratory evidence.
Nonparalytic Poliovirus Infection: Meets confirmatory laboratory evidence.
Laboratory Testing
Laboratory studies are critical for confirming whether a case of paralytic poliomyelitis is the result of wild or vaccine-related virus infection.
Refer to Chapter 22, "Laboratory Support for Surveillance of Vaccine-Preventable Diseases" for detailed information on laboratory testing for poliovirus including specific information on specimen collection and shipment.
Specimen collection
Specimen collection and shipping are important steps in obtaining laboratory diagnosis or disease confirmation. Guidelines have been published for specimen collection and handling for viral and microbiologic agents. Information is also available on using CDC laboratories as support for reference and disease surveillance; this information includes
- A central website for requesting lab testing
- The CDC Infectious Diseases Test Directory
- The form required for submitting specimens to CDC (see Appendix 23, Form # CDC 0.5034) and
Information on general requirements for shipment of etiologic agents (Appendix 24).
State laboratories and CDC provide an online test directory that contains not only a list of orderable tests for that institution, but also detailed information such as appropriate specimen types, collection methods, specimen volume, and points of contact.
Specific instructions for specimen collection and shipping may be obtained from the CDC poliovirus website or by contacting the CDC Polio/Picornavirus Laboratory at PicornaLab@cdc.gov. Because specimen submission requirements for CLIA diagnostic testing are currently being updated, ALL submissions to CDC for diagnostic testing currently require pre-approval.
Please contact PicornaLab@cdc.gov before submitting specimens to CDC. Specimens for virus identification should be sent to CDC as directed by the State Health Department.
Reporting and Case Notification
Case reporting within a jurisdiction
Each state and territory (jurisdiction) has regulations or laws governing the reporting of diseases and conditions of public health importance. 25These regulations and laws list the diseases to be reported and describe those persons or groups responsible for reporting, such as healthcare providers, hospitals, laboratories, schools, daycare and childcare facilities, and other institutions. Detailed information on notifiable conditions in each jurisdiction is available through CSTE.26 Contact your jurisdiction/state health department for reporting requirements in your jurisdiction. The Suspected Polio Case Worksheet is included as Appendix 14, to serve as a guide for data collection during the investigation of reported cases.
Case notification to CDC
Because poliomyelitis has been eliminated from the Americas, each reported case of suspected poliomyelitis should be followed up by local and state health departments in close collaboration with CDC. The jurisdiction in which the patient resides at the time of diagnosis should submit the case notification to CDC. Case notifications should not be delayed because of incomplete information or lack of confirmation; case notifications can be updated electronically as more information becomes available.
Paralytic poliomyelitis has been classified as "Immediately notifiable, Urgent," which requires that local and state health departments contact CDC within 24 hours. CDC Emergency Operations Center (770-488-7100) will provide consultation regarding the collection of appropriate clinical specimens for virus confirmation and genotyping, the initiation of appropriate consultations and procedures to rule out or confirm poliomyelitis, the compilation of medical records, and most importantly, the evaluation of the likelihood that the disease may be caused by wild or vaccine-derived poliovirus. Notifications for suspected cases of paralytic poliomyelitis should be sent to CDC using event code 10410 in the National Notifiable Disease Surveillance System (NNDSS).
Reports of nonparalytic poliovirus infection are designated as "Immediately notifiable, Urgent," which requires notification to CDC within 24 hours. CDC Emergency Operations Center (770-488-7100) will provide consultation regarding the collection of appropriate clinical specimens for confirmation and genotyping. Notifications for suspected cases of nonparalytic poliovirus infection should be sent to CDC using event code 10405 in NNDSS.
Information to collect
Demographic, clinical, laboratory, vaccination history, and epidemiologic information to determine:
- whether the suspected case meets the case definition for paralytic poliomyelitis and
- whether the disease may be caused by wild or vaccine-derived poliovirus
The following data elements are epidemiologically important and should be collected during a case investigation. See Appendix 14 for details on each data category. Additional information may be collected at the direction of the state health department or CDC.
- Demographic information
- Name
- Address
- Date of birth
- Age
- Sex
- Ethnicity
- Race
- Country of birth
- Length of time resident in the United States
- Name
- Reporting source
- County
- Earliest date reported
- County
- Clinical
- Hospitalizations: dates and duration of stay
- Date of onset of symptoms
- Complications
- Immunologic status of case-patient
- Outcome (case survived or died)
- Date of death
- Postmortem examination results
- Death certificate diagnoses
- Date of death
- Hospitalizations: dates and duration of stay
- Laboratory and clinical testing
- Stool test
- Throat swab test
- Serologic test
- Electromyogram (EMG)
- Magnetic resonance imaging (MRI)
- Stool test
- Vaccine information
- Dates and types of polio vaccination
- Number of doses of polio vaccine received
- Manufacturer of vaccine
- Vaccine lot number
- If not vaccinated, reason
- Dates and types of polio vaccination
- Epidemiological
- Recent receipt of OPV or contact with recent OPV recipient
- Is case-patient a member of a community with low vaccination coverage?
- Contact with person diagnosed with polio or poliovirus infection
- Recent receipt of OPV or contact with recent OPV recipient
Travel history
Because the last cases of paralytic poliomyelitis due to indigenously acquired wild poliovirus infection in the United States were reported in 1979, it is likely that poliovirus in a suspected case-patient is imported, either by the suspected patient directly or by a contact of the case-patient. Results of differentiation tests may not be available at the time of the case investigation. Therefore, to rule out the possibility of imported wild poliovirus, or an imported vaccine-derived poliovirus, a detailed travel history of suspected cases and of other household and non-household contacts should be obtained. Any resident of, recent travel to, or contact with visitors from geographic areas where risk of polio is elevated or OPV is used might be particularly revealing.
Communities
Because communities with low vaccination coverage327 are at increased risk of poliomyelitis when a poliovirus is introduced into the population, a suspected case of poliomyelitis reported from an undervaccinated population should be assigned the highest priority for follow-up and collection of specimens.
Vaccination
For specific information about poliovirus vaccination, refer to The Pink Book, which provides general recommendations, including vaccine use and scheduling, immunization strategies for providers, vaccine content, adverse events and reactions, vaccine storage and handling, and contraindications and precautions.
Enhancing Surveillance
A number of activities can improve the detection and reporting of cases and improve the comprehensiveness and quality of reporting. Additional surveillance activities are listed in Chapter 19, "Enhancing Surveillance."
Promoting awareness
Because of the severity of poliomyelitis disease, clinicians are often the first to suspect the diagnosis of poliomyelitis and are the key to timely reporting of suspected cases. However, disease notification by clinicians is often delayed because it is only after other differential diagnoses are ruled out that the diagnosis of poliomyelitis is considered. Encouraging surveillance for acute flaccid myelitis (AFM), which presents with acute onset of flaccid limb weakness and at least some gray matter involvement in the spinal cord, and is clinically similar to poliomyelitis disease, can also be used to promote physicians’ awareness of the importance of prompt notification of suspected cases of both polio and AFM to the state and local health department and CDC and of the need to obtain stool and throat specimens early in the disease course.
Ensuring laboratory capabilities
Make sure that the state laboratory or other easily accessible laboratory facility can perform, at a minimum, enterovirus molecular typing (PCR plus sequencing of the VP1 genome region). The CDC polio laboratory is always available for consultation and/or testing.
Obtaining laboratory confirmation
Appropriate stool and throat specimens (2 specimens taken at least 24 hours apart during the first 14 days after onset of paralytic disease) should be collected and sent to the CDC polio laboratory for confirmation and to differentiate between possible wild-type or vaccine-derived strains.
Active surveillance
Active surveillance should be conducted for every confirmed case of poliomyelitis to ensure timely reporting. The diagnosis of a case of poliomyelitis, particularly in a member of a group that refuses vaccination, should prompt immediate control measures as well as active surveillance activities. These activities should include active contact tracing among populations at risk.
Case Investigation
Timely collection of stool specimens is important in establishing the diagnosis and determining appropriate control measures. In the event of poliovirus detection, refer to the poliovirus website for specific information on specimen collection and testing.
Guidelines and a worksheet for the investigation of suspected cases of poliomyelitis are included as Appendix 14. Suspected cases of poliomyelitis should be reported immediately to the state health department. CDC's Emergency Operations Center should also be contacted at 770-488-7100.
- Paralytic poliomyelitis — United States, 1980–1994. MMWR Morb Mortal Wkly Rep 1997;46(4):79–83.
- Prevots DR, Sutter RW, Strebel PM, et al. Completeness of reporting for paralytic polio, United States, 1980–1991. Arch Pediatr Adolesc Med 994;148(5):479–85. doi: 10.1001/archpedi.1994.02170050037007.
- Strebel PM, Sutter RW, Cochi SL, et al. Epidemiology of poliomyelitis in the United States one decade after the last reported case of indigenous wild virus-associated disease. Clin Infect Dis 1992;14(2):568–79. doi: 10.1093/clinids/14.2.568.
- Poliomyelitis prevention in the United States: introduction of a sequential vaccination schedule of inactivated poliovirus vaccine followed by oral poliovirus vaccine: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 1997;46(RR-3):1–25.
- Poliomyelitis prevention in the United States: updated recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2000;49(RR-5):1–22.
- Recommended childhood immunization schedules for persons aged 0 through 18 years — United States, 2010. MMWR Morb Mortal Wkly Rep 2010;58(51):1–4.
- American Academy of Pediatrics Committee on Infectious Diseases. Prevention of poliomyelitis: recommendations for use of only inactivated poliovirus vaccine for routine immunization. Pediatrics 1999;104(6):1404–6
- Imported vaccine-associated paralytic poliomyelitis—United States, 2005. MMWR Morb Mortal Wkly Rep 2006;55(4):97–9.
- DeVries AS, Harper J, Murray A, Lexau C, et al. Vaccine-derived poliomyelitis 12 years after infection in Minnesota. N Engl J Med 2011;364(24):2316–23.
- Trimble R, Atkins J, Quigg TC, Burns CC et al. Vaccine-associated paralytic poliomyelitis and BCG-osis in an immigrant child with severe combined immunodeficiency syndrome—Texas, 2013. MMWR Morb Mortal Wkly Rep 2014;63(33):721–4.
- World Health Assembly. Global eradication of poliomyelitis by the year 2000. [resolution no. WHA41.28]. Geneva, Switzerland: World Health Organization;1988.
- Sutter R, Kew O, Cochi S, et al. Poliovirus vaccine—live. In Plotkin S, Orenstein W, Offit P editors. Plotkin's Vaccines. 7th ed. Philadelphia, PA: Elsevier;2018:866–917.
- Chard AN, Datta SD, Tallis G, et al. Progress toward polio eradication—worldwide, January 2018–March 2020. MMWR Morb Mortal Wkly Rep 2020;69:784–9. doi: http://dx.doi.org/10.15585/mmwr.mm6925a4external icon
- Davlantes E, Greene SA, Tobolowsky FA, et al. Update on wild poliovirus type 1 outbreak—Southeastern Africa, 2021–2022. MMWR Morb Mortal Wkly Rep 2023;72:391–7. doi: http://dx.doi.org/10.15585/mmwr.mm7215a3
- Update: outbreak of poliomyelitis—Dominican Republic and Haiti, 2000–2001. MMWR Morb Mortal Wkly Rep 2001;50(39):855–6.
- Modlin JF. The bumpy road to polio eradication. N Engl J Med. 2010;362(25):2346–9. doi: 10.1056/NEJMp1005405.
- Immunization Systems Management Group of the Global Polio Eradication Initiative. Introduction of inactivated poliovirus vaccine and switch from trivalent to bivalent oral poliovirus vaccine—worldwide, 2013–2016. MMWR Morb Mortal Wkly Rep 2015; 64(25):699–702.
- World Health Organization. Report of the Meeting of the WHO Global Advisory Committee on Vaccine Safety, 15-16 May 2023. Wkly Epidemiol Rec (2023);98(32):345–54.
- Wallace GS, Curns AT, Weldon WC, Oberste, MS. Seroprevalence of poliovirus antibodies in the United States population, 2009–2010. BMC Public Health 2016;16:721. doi: 10.1186/s12889-016-3386-1.
- Wallace GS, Pahud BA, Weldon WC, et al. Seroprevalence of poliovirus antibodies in the Kansas City metropolitan area, 2012–2013. Hum Vaccin Immunother. 2017:13(4):776–83. doi: 10.1080/21645515.2016.1255386.
- Chen RT, Hausinger S, Dajani A, et al. Seroprevalence of antibody against poliovirus in inner-city preschool children: implications for vaccination policy in the United States. JAMA 1996:275(21):1639–45. doi:10.1001/jama.1996.03530450029028.
- Hill HA, Chen M, Elam-Evans LD, Yankey D, Singleton JA. Vaccination coverage by age 24 months among children born during 2018–2019 — National Immunization Survey–Child, United States, 2019–2021. MMWR Morb Mortal Wkly Rep 2023;72:33–8. doi: http://dx.doi.org/10.15585/mmwr.mm7202a3.
- Link-Gelles R, Lutterloh E, Schnabel Ruppert P, et al. Public health response to a case of paralytic poliomyelitis in an unvaccinated person and detection of poliovirus in wastewater—New York, June–August 2022. MMWR Morb Mortal Wkly Rep 2022;71:1065–8. doi: http://dx.doi.org/10.15585/mmwr.mm7133e2.
- Update to public health reporting and national notification for paralytic poliomyelitis and nonparalytic poliovirus infection. Atlanta, GA: CSTE; 2023.
- Roush S, Birkhead G, Koo D, Cobb A, Fleming D. Mandatory reporting of diseases and conditions by health care professionals and laboratories. JAMA 1999;282(2):164–70. doi:10.1001/jama.282.2.164.
- State reportable conditions websites. Atlanta, GA: CSTE; Accessed 2023 September 7.
- Foote FM, Kraus G, Andrews MD, et al. Polio outbreak in a private school. Conn Med 1973:37(12):643–4.
