What to know
This Steps to Better Health fact sheet provides easy-to-read information for people with sickle cell disease (SCD) about blood transfusion safety.

Overview
If you have sickle cell disease (SCD), you may need one or more blood transfusions (healthy blood from a donor put into your body) during your lifetime. During a blood transfusion, your blood and the donated blood must have matching antigens, or special proteins on the surface of each red blood cell.
If the antigens in your blood and the donated blood do not match, your immune system (your body's ability to fight germs) may attack the new blood. This transfusion reaction can cause serious health problems. Below are steps you can take for safer blood transfusions.
Share Your Transfusion History with Your Healthcare Provider
Share past health information including your number of lifetime transfusions and any reactions to blood transfusions such as severe pain, fatigue, brown or red urine, and fever. If you have had past transfusion reactions, your provider may talk to you about the risks and benefits of immunosuppressants. These medicines lower the chance of your immune system rejecting the donor blood, protecting you from a life-threatening transfusion reaction.
Know Your Blood Type
Ask your provider for an extended red cell antigen profile, a test that determines your antigens. Share the results with your healthcare providers before your blood transfusion.
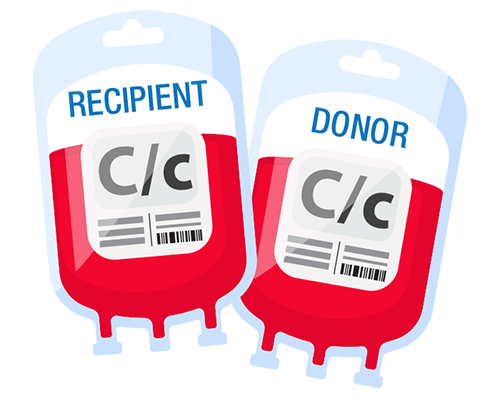
Request Blood Matching
Once you know your antigens, they need to be matched with the antigens of the donor's blood to avoid a transfusion reaction during the blood transfusion. Ask your provider for blood that is matched for these antigens to which people with SCD most commonly have transfusion reactions: C/c, E/e, and K red cell antigens.
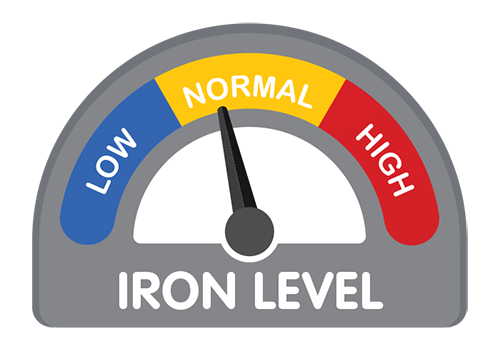
Track Your Iron Levels
If you have received more than 10 transfusions in your lifetime, you may be at risk for iron overload (too much iron in the body). Ask your provider for a ferritin blood test, which measures the amount of iron in your blood. If your ferritin levels are high (greater than 1,000) and you receive transfusions on a regular schedule, your provider should run a magnetic resonance imaging (MRI) test that measures iron levels in your liver. Your provider may also run an MRI that measures iron levels in your heart.
Talk to Your Provider About Your Transfusion Options
If you need regular transfusions, ask your provider about an automated red cell exchange, a transfusion process that removes and replaces sickled cells with healthy blood. This process may be preferred over a simple blood transfusion during which healthy blood is added to blood with sickled cells. An automated red cell exchange can lower your risk for health problems, such as iron overload.
Learn more about blood transfusions here.
This information is based on ASH SCD Guidelines: Transfusion support.
