What to know
- Rubella IgG serology testing should be used for assessing rubella immunity, including before, during, and after pregnancy.
- Testing for rubella IgG avidity can be used to distinguish between recent exposure to rubella and a more distant exposure.
- Rubella IgM testing should be limited to suspected rubella cases. It is not recommended for screening asymptomatic people.
- Routine IgM screening of pregnant people is not recommended.
- No fetal testing is recommended.
IgM vs. IgG serology testing
Rubella-virus specific IgM antibodies (rubella IgM) develop shortly after primary infection or vaccination. Rubella-virus specific IgG antibodies (rubella IgG) become detectable by day four after rash onset in rubella infections and reach peak levels in the following one to two weeks. While rubella IgM persists for up to three months, rubella IgG can last a lifetime.
Although rubella was officially declared to be eliminated from the United States in 2004, ongoing rubella activity in many other countries can result in imported sporadic U.S. cases or outbreaks.
Serum sample collection
Detection of specific IgM antibodies in a serum sample collected within the first few days after rash onset can provide presumptive evidence of a recent rubella virus infection. The optimum time-point for collection of serum is five days after the onset of symptoms (fever and rash) when >90% of cases will be IgM positive.
On the day of rash onset only about 50% of cases are IgM positive. Therefore, if serum that collected less than five days after onset is negative, a second sample would be necessary to confirm or rule out rubella. When CDC receives serum samples to test for clinically suspected rubella, CDC also determines the anti-rubella IgM or IgG status for each sample to aid in case classification. The interpretation of rubella laboratory results must always take into account relevant clinical and epidemiological data.
IgG avidity testing
Since no assay is 100% specific, serology testing of non-rubella cases occasionally produces false positive IgM results. In the United States where endemic circulation of wild-type rubella virus has been eliminated and the chance of contracting the disease domestically is low, most suspected cases are not rubella.
Rash and fever illnesses are more likely due to a number of other rash–causing illnesses such as parvovirus B19, enteroviruses such as coxsackieviruses and echoviruses, or human herpesvirus–6 (roseola). The presence of rheumatoid factor can also result in a false positive IgM. Due to the possibility of false positive results, IgM should not be included in routine testing to determine evidence of prior rubella immunity.
It is important to distinguish IgM reactivity caused by primary infection from that caused by IgM persistence or cross-reactivity with other antigens, especially in pregnant people.
Measurement of rubella IgG antibody avidity
The measurement of rubella IgG antibody avidity can be used to distinguish between recent exposure to rubella and more distant rubella exposure. Antibody avidity (the overall strength of binding between the antigen and antibody) increases with time; this is known as maturation of the immune response. As the immune response matures, low avidity antibodies are replaced with high avidity antibodies.
Avidity differences can be detected by using protein denaturants such as diethylamine (DEA) in the washing step of an enzyme-linked immunoassay (EIA) for rubella IgG.
- Low avidity rubella IgG suggests recent infection and can be detected for up to four months after infection.
- High avidity rubella IgG suggests a more distant rubella exposure, which may be from either via infection or vaccination.
The cut-off between low and high avidities has to be established by using standardized sera and a particular EIA kit.
Testing pregnant patients
IgG serology testing for rubella immunity
Detection of rubella IgM by enzyme immunoassay (EIA) is used to confirm suspected cases of acute rubella infection and congenital rubella syndrome (CRS). IgM is typically detectable between 4 and 30 days after rash onset in acute rubella infection and for up to six months after birth in CRS cases. A person may also be rubella IgM positive after recent vaccination.
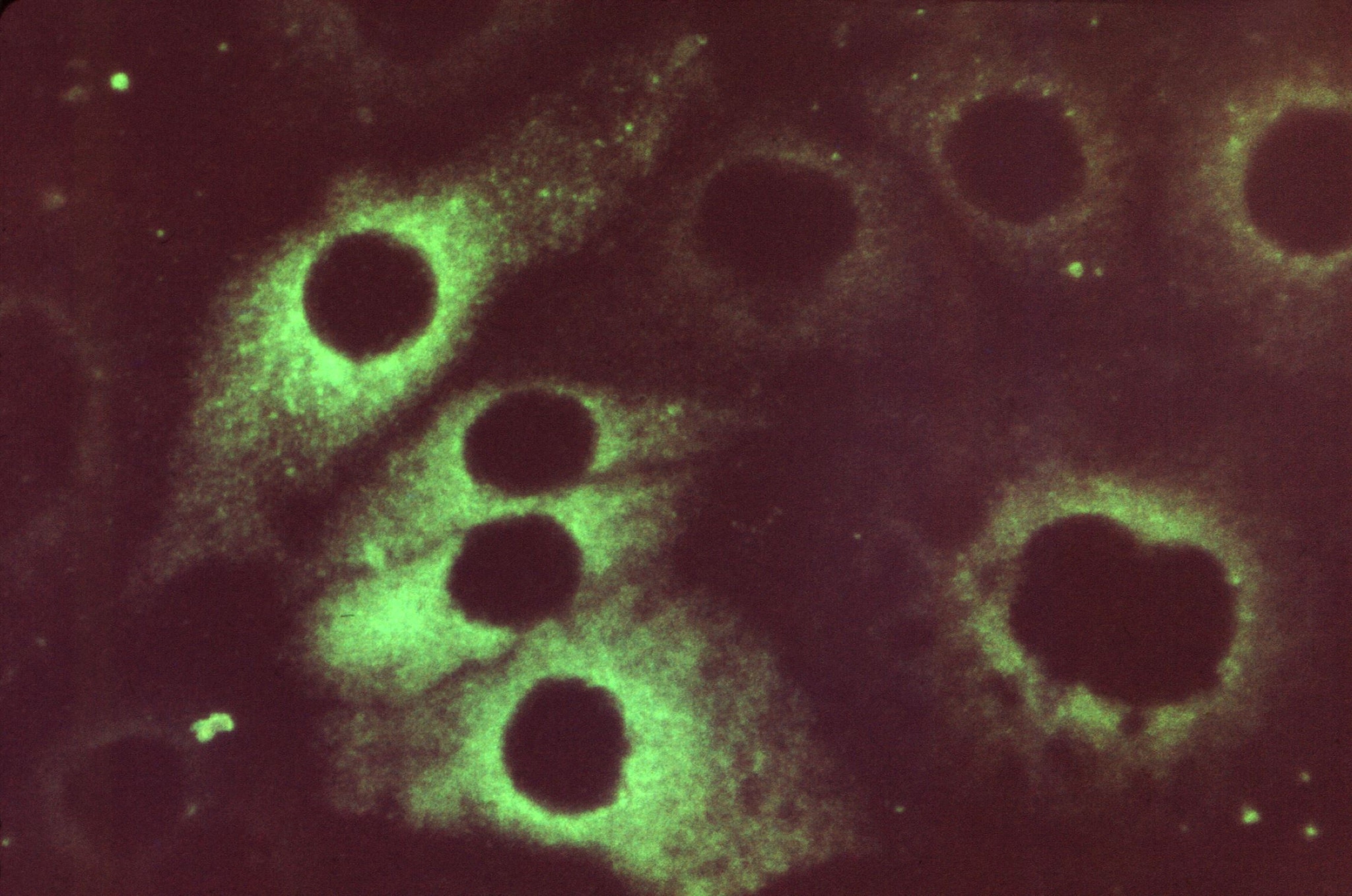
Detection of rubella IgG by EIA
Detection of rubella IgG by EIA is used to assess immunity to rubella. EIA can reliably detect rubella IgG concentrations greater than 10 IU/ml, which is the cutoff for defining rubella immunity used in the United States. Rubella IgG serology testing should be used for assessing rubella immunity before, during, and after pregnancy.
Routine IgM screening is not recommended
Routine IgM screening of pregnant people is not recommended. Rubella IgM testing in asymptomatic, unexposed pregnant people is inappropriate because false positive results can occur, which can be misleading. Rubella IgM testing in pregnant people should be limited to suspected rubella cases. However, providers sometimes inappropriately order IgM tests to assess rubella immunity.
Serology testing recommendations for CRS
Rubella is very dangerous during pregnancy
CRS was eliminated from the United States in 2004, but cases can still be imported by pregnant people who contract rubella in an endemic country. In rare cases, CRS can occur in the United States when susceptible pregnant people are exposed to confirmed rubella cases.
CRS cases can be diagnosed in newborns and young infants using detection of rubella IgM. Suspected cases should be tested as close to birth as possible and again at 1 month of age if the initial IgM test is negative. If paired sera are to be collected, the second sample should be collected 14 to 21 days after the acute specimen was collected. At 3 months of age, approximately 50% of cases would still have detectable rubella IgM in their serum. Additionally, the presence of rubella IgG in an infant after the decline of maternal antibodies (9 months of age) and the absence of vaccination or exposure to rubella will confirm CRS.
Other rubella tests for pregnant patients
IgM capture EIA
If IgM testing is inappropriately performed and an IgM positive result is obtained for an asymptomatic pregnant patient with no history of rubella exposure, the IgM positive result should be confirmed by retesting in a different laboratory with a different EIA test format. Preferably, testing should be performed by an IgM capture EIA because IgM capture assays are more specific than indirect IgM EIA assays.
Early IgG avidity testing
Testing for rubella IgG avidity can be used to distinguish between recent exposure to rubella and a more distant exposure. Avidity testing is most useful in early pregnancy to help rule out a rubella infection in the first trimester, when the risk of congenital defects due to rubella is highest. It is not as useful in late pregnancy because avidity will be high by the third trimester if infection occurred in the first trimester.
RT-PCR assay
Rubella reverse transcription polymerase chain reaction (RT-PCR) assay can also be used to confirm acute rubella infection, but its utility is limited because of the narrow window when the virus can be detected in clinical samples in acquired rubella cases. In respiratory samples, rubella RNA is typically detectable from two days before rash onset to four days after rash onset. In elimination settings, the positive predictive value of rubella RT-PCR in a respiratory sample from an asymptomatic, IgM-positive pregnant patient is low.
Currently used rubella RT-PCR assays have not been validated for testing amniotic fluid or other fetal specimens and should not be used for confirmation of suspected CRS. Although amniotic fluid has been considered for detection of rubella RNA by RT-PCR when fetal infection is suspected, the sensitivity of this method is less than 86%, particularly before the 21st week of gestation. RT-PCR assays on throat swabs, nasopharyngeal swabs, and urine specimens from a neonate are used for confirmation of suspected CRS cases.
- Bouthry E, Perillaud-Dubois C, Lebraud P, Soutiere MP, Grangeot-Keros L, Vauloup-Fellous C. Positive predictive value of seroconversion or positive rubella IgM in diagnosis of maternal rubella infection: Seven-years review of French National Reference Laboratory for Rubella. J Clin Virol. 2021;134:104708.
- Colman S, Vernelen K, China B, Van den Bossche D, Cornelissen L, Delforge ML, et al. Pitfalls of rubella serology while on the brink of elimination: evaluation of national data, Belgium, 2017. Euro Surveill. 2021;26(20).
- Hiebert J, Zubach V, Charlton CL, Fenton J, Tipples GA, Fonseca K, et al. Evaluation of diagnostic accuracy of eight commercial assays for the detection of rubella virus specific IgM antibodies. J Clin Microbiol. 2021:JCM0159721.
- Isaac BM, Zucker JR, Giancotti FR, Abernathy E, Icenogle J, Rakeman JL, et al. Rubella Surveillance and Diagnostic Testing among a Low-Prevalence Population, New York City, 2012-2013. Clin Vaccine Immunol. 2017;24(9).
- Best J, Enders G. Laboratory diagnosis of rubella and congenital rubella. In: Banatvala JE, Peckham CS, editors. Rubella Viruses. Perspectives in Medical Virology. 15. London: Elsevier; 2007. p. 39-77.
- Vauloup-Fellous C, Grangeot-Keros L. Humoral immune response after primary rubella virus infection and vaccination. Clin Vacc Immunol 2007;14(5):644-7.
- Tanemura M, Suzumori K, Yagami Y, Katow S. Diagnosis of fetal rubella infection with reverse transcription and nested polymerase chain reaction: a study of 34 cases diagnosed in fetuses. Am J Obstet Gynecol. 1996;174(2):578-82.
