Volume 11 — November 13, 2014
ORIGINAL RESEARCH
Evolution in Obesity and Chronic Disease Prevention Practice in California Public Health Departments, 2010
Navigate This Article
Liz Schwarte, MPH; Samantha Ngo, BA; Rajni Banthia, PhD; George Flores, MD, MPH; Bob Prentice, PhD; Maria Boyle, MS, RD; Sarah E. Samuels, DrPH†
†Deceased.
Suggested citation for this article: Schwarte L, Ngo S, Banthia R, Flores G, Prentice B, Boyle M, et al. Evolution in Obesity and Chronic Disease Prevention Practice in California Public Health Departments, 2010. Prev Chronic Dis 2014;11:120177. DOI: http://dx.doi.org/10.5888/pcd11.120177.
PEER REVIEWED
Abstract
Introduction
Local health departments (LHDs) are dedicating resources and attention to preventing obesity and associated chronic diseases, thus expanding their work beyond traditional public health activities such as surveillance. This study investigated practices of local health departments in California to prevent obesity and chronic disease.
Methods
We conducted a web-based survey in 2010 with leaders in California’s LHDs to obtain diverse perspectives on LHDs’ practices to prevent obesity and chronic disease. The departmental response rate for the 2010 survey was 87% (53 of California’s 61 LHDs).
Results
Although staff for preventing obesity and chronic disease decreased at 59% of LHDs and stayed the same at 26% of LHDs since 2006, LHDs still contributed the same (12%) or a higher (62%) level of effort in these areas. Factors contributing to internal changes to address obesity and chronic disease prevention included momentum in the field of obesity prevention, opportunities to learn from other health departments, participation in obesity and chronic disease prevention initiatives, and flexible funding streams for chronic disease prevention. LHDs that received foundation funding or had a lead person or organizational unit coordinating or taking the lead on activities related to obesity and chronic disease prevention were more likely than other LHDs to engage in some activities related to obesity prevention.
Conclusion
California LHDs are increasing the intensity and breadth of obesity and chronic disease prevention. Findings provide a benchmark from which further changes in the activities and funding sources of LHD chronic disease prevention practice may be measured.
Introduction
Local health departments (LHDs) dedicate resources and attention to preventing obesity and chronic disease (1), thus expanding their work beyond traditional public health activities such as disease surveillance and control to increasing access to healthful food and physical activity. This work occurs particularly in lower income communities of color where obesity and chronic disease rates are highest. This approach parallels research demonstrating that environmentally focused interventions to prevent obesity and chronic disease have a greater impact than individual behavior modification approaches (2,3). LHDs can play a leadership role in promoting these interventions (4–6); however, little is known about LHDs’ capacities for expanding their work to prevent obesity and chronic disease. Given high obesity and chronic disease rates (7), growing momentum in the field of chronic disease prevention, and the fiscal crises counties face (8), it is crucial to monitor LHDs’ abilities to maintain and deepen activities for preventing obesity and chronic disease.
The Sarah Samuels Center for Public Health Research and Evaluation conducted a survey of California LHDs in 2007 (Phase I) to understand their capacity, practices, and resources for changing nutrition and physical activity environments for preventing obesity and chronic disease (5). Samuels Center conducted a second survey in 2010 (Phase II) to understand how LHD practice had changed since the Phase I survey, hypothesizing that LHD capacities had evolved to meet the increasing need for interventions to prevent obesity and chronic disease. Phase II was also designed to learn whether foundation funding and a lead person or organizational unit for preventing obesity and/or chronic disease influences LHDs’ activities to improve nutrition and physical activity environments.
California’s LHD practice has matured to encompass community and governmental collaborations, practice equity, and regional approaches. For many LHDs, obesity prevention was the gateway through which practice has expanded to address chronic disease prevention and underlying conditions that affect health. The Phase II survey was conducted to learn about LHDs’ readiness and capacity to progress along this continuum and to provide a benchmark from which to measure the evolution of public health practice for preventing obesity and chronic disease. We present Phase II survey findings.
Methods
Sample
We contacted 175 staff members in California’s 61 county health departments, including public health directors, health officers, nutrition managers, chronic disease prevention directors, and obesity and chronic disease prevention coordinators and invited them to participate in the Phase II survey, which was conducted in 2010. We identified potential respondents through professional associations, Internet searches, e-mails, and telephone calls. These professional groups were selected because of the pivotal role they play in LHDs in preventing obesity and chronic disease, and to obtain diverse perspectives within LHDs. The number of respondents per department ranged from 1 to 6 and was typically 1 (mode).
Survey measures
The Samuels Center, in collaboration with the Partnership for the Public’s Health, the Public Health Institute, and The California Endowment, developed the Public Health Departments and Obesity/Chronic Disease Prevention Phase II Survey. Survey questions assessed 1) how LHDs are working to change nutrition and physical activity environments to prevent obesity and chronic disease and 2) which factors influence their activities. We refined questions from the Phase I survey to enhance their relevance to public health practice evolution and added new questions. Although the Phase I survey focused only on obesity prevention, Phase II focused also on chronic disease prevention. We adapted environmental and policy change items from the Institute of Medicine’s (IOM’s) Local Government Actions to Prevent Childhood Obesity report (9). The survey contained 24 items and took 10 minutes to complete. The Public Health Institute Institutional Review Board determined that no review was necessary for this research. We used a web-based survey tool to administer the survey.
Data analysis
We exported data from the web-based tool into SPSS (IBM, Inc) and analysed the LHD-level data by aggregating individual respondents’ answers to each question for each department. For yes/no questions, if at least 1 respondent from each LHD answered yes, we assigned an affirmative response to the department. For scaled questions, we averaged individual responses from each department. We grouped responses by whether LHDs received philanthropic foundation grant funding and by whether LHDs had a lead person or organizational unit for preventing obesity and chronic disease.
Results
At least 1 individual responded to the survey in 53 of California’s 61 LHDs, equaling an 87% departmental response rate. The 53 LHDs that did respond serve nearly all (99.5%) of California’s population of 37 million (10). We asked respondents to self-identify their position: 27% were program managers for nutrition or the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), 23% were public health officers, 15% were public health directors, 4% were chronic disease directors, and 2% were physical activity managers. The remaining respondents fell into the category of “other” staff (29%), including deputy directors, health promotion managers, and nutritionists.
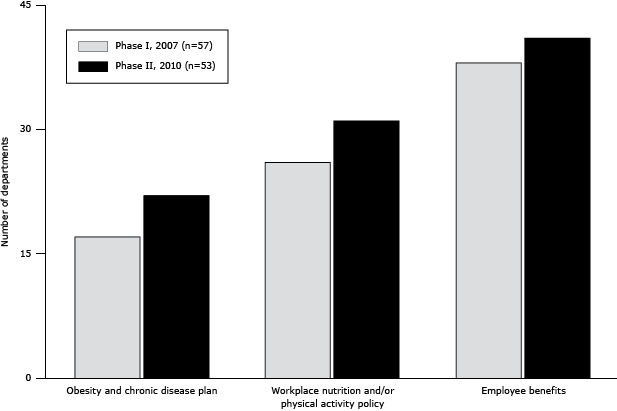
Organizational plans and worksite policies
Twenty-two LHDs in Phase II either had an organizational plan for preventing obesity and chronic disease or participated in a county-wide plan, compared with 17 departments in Phase I (Figure). Thirty-one LHDs had workplace nutrition policies, physical activity policies, or both for their own staff, an increase of 5 from Phase I. Forty-one LHDs also had employee benefit programs encouraging employees to engage in physical activity such as wellness programs, fitness club discounts, and walking clubs, 3 more than in Phase I.
Figure. Obesity and chronic disease prevention plans and policies in local public health departments, by study phase, California Public Health Departments Obesity and Chronic Disease Prevention Survey, 2007 and 2010. [A tabular version of this figure is available.]
Staff capacity
In 72% (n = 38) of LHDs, there was a lead person or organizational unit for preventing obesity and chronic disease. At those organizational units, activities included health promotion (21%), community health (16%), chronic disease prevention (16%), and health policy (3%). Although most departments either lost staff (59%) or had the same number of staff (26%) as in 2006, many departments increased their effort (62%) or put about the same effort (12%) into preventing obesity and chronic disease.
Respondents ranked their capacity (knowledge, skills, and/or expertise) for preventing obesity and chronic disease on a rating scale (1, poor/none; 2, fair; 3, good; 4, excellent). LHDs, on average, reported that they have good or excellent capacity for nutrition-related activities. They ranked providing access to healthful food, communications, community organizing, intersectoral collaboration, and leadership capacities as good. LHDs reported having fair research capacity, urban planning/community design/transportation capacity, and violence prevention capacity, and fair or poor/none legal expertise. The barriers most commonly cited for being unable to engage in activities related to preventing obesity and chronic disease were limited training (45%) and salaries too low to attract quality staff (19%).
Strengthening focus
In the 4 years preceding the survey, 74% (n = 39) of the departments had changed internally in 1 or more ways to address obesity and chronic disease prevention. Over half (53%) of LHDs had reorganized internally; 51% had implemented nutrition and physical activity policies and programs. Nearly half of the departments had trained staff (47%) and increased leadership (45%).
Of 39 LHDs indicating internal changes, 77% attributed changes to increased momentum in the field of obesity prevention (Table 1). LHDs also attributed change to other contributors: regional and statewide efforts in preventing obesity and chronic disease (67%); learning from other health departments (59%); and obesity prevention initiatives such as Healthy Eating, Active Communities (HEAC), Central California Regional Obesity Prevention Program (CCROPP), and the public health department mini-grants program (46%).
Funding sources
Almost two-thirds of LHDs used WIC funding for preventing obesity and chronic disease, followed by realignment (funding from the transfer of program responsibility and revenue sources for sales tax and vehicle license fees from the state to counties) (60%) and Title V (Maternal, Child, and Adolescent Health) funding (57%) (Table 2). LHDs that received foundation funding were more likely than LHDs without foundation funds to use local general funds (69%) and Network for a Healthy California funds (75%) as additional resources for preventing obesity and chronic disease.
Engagement in activities
All responding LHDs engaged in at least 1 of the IOM’s recommended environmental and policy change activities to prevent childhood obesity. Whether they received foundation funds or had a lead or organizational unit for preventing obesity and chronic disease influenced how likely they were to engage in certain activities (Table 3).
Over half of LHDs engaged in built environment assessment activities (57%) and geographic information system (GIS) mapping (51%). LHDs that received foundation funding were more likely than LHDs without foundation funds to conduct built environment studies (81% vs 33%), Communities of Excellence (CX3) (73% vs 22%), GIS mapping (65% vs 37%), and health impact assessments (46% vs 7%). Similarly, LHDs with a lead for preventing obesity and chronic disease were more likely than LHDs without a lead to perform built environment assessments (76% vs 7%), CX3 (61% vs 13%) assessments, and GIS mapping (63% vs 20%).
Eighty-three percent of LHDs participated in planning commissions or committees focused on improving the built environment, and 60% collaborated with other health departments in regional obesity prevention efforts. LHDs with foundation funding were more likely than LHDs without foundation funds to participate in school or community collaboratives or coalitions (92% vs 82%) or engage in preventing obesity and chronic disease through collaboration with other health departments (85% vs 37%). LHDs with a lead for preventing obesity and chronic disease were more likely than LHDs without a lead to be involved in school or community collaboratives or coalitions (90% vs 80%) and planning commissions or committees (92% vs 60%).
Forty-two percent of LHDs worked with schools to enforce state physical education requirements, and 30% worked toward ensuring free and safe drinking water availability. More LHDs with a lead for preventing obesity and chronic disease than LHDs without a lead worked to improve food and beverage environments (76% vs 20%), state physical education requirement enforcement (50% vs 20%), and drinking water availability (40% vs 7%).
Many LHDs helped small store owners carry more healthful, affordable items (42%), and limited fast food accessibility through zoning or policy measures (23%). More LHDs that received foundation funding helped store owners carry more healthful items than did LHDs without foundation funds (69% vs 15%). LHDs with a lead for preventing obesity and chronic disease were more likely to help store owners carry more healthful items (58% vs 0%), support incentive programs or use zoning laws to attract grocery stores to underserved neighborhoods (42% vs 0%), and limit fast food access (32% vs 0%) than LHDs without a lead.
To increase community food access, LHDs encouraged federal food assistance program acceptance at farmers markets (72%), monitored menu labeling in chain restaurants and/or encouraged nonchain restaurants to provide calorie information (28%), and offered incentives to restaurants that provide healthier options (13%). LHDs that received foundation funding were more likely than LHDs without foundation funds to promote food assistance program acceptance at farmers markets (92% vs 52%), farmers markets establishment (85% vs 48%), menu labeling (46% vs 11%), and incentives to restaurants that offer healthier options (27% vs 0%). LHDs with a lead for preventing obesity and chronic disease were more likely to promote food assistance program acceptance at farmers markets (82% vs 47%), farmers markets establishment (82% vs 27%), and monitoring menu labeling (37% vs 7%) than LHDs without a lead.
Forty-two percent of LHDs supported public venue and worksite nutrition standards and/or physical activity guidelines. LHDs that received foundation funding were more likely than LHDs that did not receive foundation funding to support nutrition and/or physical activity guidelines for worksites (73% vs 11%) and public venues (58% vs 26%). More LHDs with a lead than LHDs without a lead for preventing obesity and chronic disease supported nutrition and/or physical activity guidelines for worksites (58% vs 0%) and public venues (55% vs 7%).
Overall, 68% of LHDs supported sidewalk planning and building, and 60% developed and implemented Safe Routes to School programs with schools. LHDs that received foundation funding were much more likely than LHDs without foundation funds to engage in sidewalk planning and building (89% vs 48%), Safe Routes to Schools (85% vs 37%), and joint use agreements (69% vs 30%). Similarly, LHDs with a lead for preventing obesity and chronic disease collaborated on physical activity improvements at a much higher rate than LHDs without a lead; 87% of those with a lead and 20% of those without a lead worked on sidewalk planning and building. Of LHDs with a lead, 76% worked on Safe Routes to School (compared with 20% without a lead), 63% worked on joint use agreements (compared with 13% without a lead), and 66% supported park development (compared with 20% without a lead).
Discussion
Agents for change
The Phase II survey findings show that LHDs, in collaboration with local governments and community leaders, are agents of change for preventing obesity and chronic disease. As a new standard of practice, California LHDs are addressing the policies, systems, and environments that underpin good health-related outcomes.
LHDs made changes within their organizations for preventing obesity and chronic disease through reorganization, reallocation of resources, leadership development and staff training, and nutrition and physical activity policy implementation. An important finding is that LHDs attribute their organizational and practice changes to contextual factors such as learning from regional and state obesity and chronic disease prevention efforts, learning from other LHDs, and participating in obesity prevention initiatives. LHDs also favorably rated their staffs’ capacity in various skill areas needed for preventing obesity and chronic disease, demonstrating that departments are reshaping their organizations. These findings may explain why LHDs can report both increasing their efforts for preventing obesity and chronic disease and losing or maintaining the same staff or resources to support these activities.
LHDs relied on and used both governmental and foundation funding for preventing obesity and chronic disease. Foundation funding, which may allow LHDs more flexibility than governmental funding in how the funds are used, appears to have provided impetus for California LHDs to engage in changing nutrition and physical activity environments. These findings are consistent with findings from Phase I (5). More than 70% had a lead person or division for preventing obesity and chronic disease, which is consistently associated with pursuing environmental and policy approaches for preventing obesity and chronic disease.
Evolution in practice
Public health practice in California changed considerably since our first survey in 2007. Key developments were the position paper issued by the California Conference of Local Health Officers (CCLHO) (11) in 2007 and regional workshops in 2008 to strengthen department capacity for preventing obesity and chronic disease. Additionally, the Bay Area Regional Health Inequities Initiative convened 11 LHDs to transform public health practice so as to change conditions that contribute to health disparities and cultivate recognition that social justice and equity are at the heart of reducing conditions that fuel the obesity and chronic disease epidemics (12).
Activities for preventing obesity and chronic disease gained visibility and momentum through HEAC and CCROPP — pioneering, multisector initiatives to change nutrition and physical activity environments in low-income, ethnically diverse communities. These programs achieved full implementation between Phase I and Phase II, and may explain the high level of LHD engagement in policy, systems, and environmental approaches to prevent obesity and chronic disease. Fourteen LHDs played major roles in the 2 initiatives (13–16).
Change in policy and systems at the state level further fueled momentum in LHDs to improve nutrition and physical activity environments in California. A Health in All Policies Task Force (convened by The California Department of Public Health) was created to foster collaboration between California state departments and to require consideration of the health impact of all proposed policies (17).
Although LHDs worked on preventing obesity and chronic disease with fewer resources and staff in an already challenging funding environment (18–20), new federal funding sources and sustained leadership from the public health profession have bolstered efforts. Under the federal American Recovery and Reinvestment Act of 2009, the California Department of Public Health and 3 LHDs received Communities Putting Prevention to Work (CPPW) cooperative agreements to reduce chronic disease through changes in policy, systems, and environment (21). At the time the survey was conducted, CPPW resources had not yet been awarded in California. Anticipation of these resources may have stimulated LHDs’ interest and activity in community-level chronic disease prevention and influenced survey responses. The Affordable Care Act supported Community Transformation Grants (CTGs) (22), which were awarded to 9 California LHDs to address tobacco-free living, active living and healthful eating, and clinical and other preventive services. A state CTG awarded to the Public Health Institute in collaboration with the California Department of Public Health covers implementation in 42 counties, with 12 LHDs receiving direct funding. CPPW and CTGs built on an LHD and community collaboration model catalyzed by the Partnership for the Public’s Health (23) and expanded on by HEAC and CCROPP to address policy and environmental change for obesity prevention across sectors.
In concert with the influx of CPPW and CTG resources into California LHDs, 10 LHDs representing 64% of the state’s population formed the Public Health Alliance of Southern California (formerly Southern California Chronic Disease Collaborative) in 2012 to address chronic disease prevention regionally through multisector policy, environmental, and systems change (T. Delaney, PhD, RD, oral communication, March 2013). The CCLHO and the County Health Executives Association of California, professional organizations representing LHDs, are jointly developing a Chronic Disease Prevention Framework to advance a common chronic disease prevention agenda in California locally and statewide (24).
The Affordable Care Act’s Prevention and Public Health Fund (25) provides unprecedented resources and models for addressing chronic disease prevention and fostering new links between LHDs and medical care as well as health workforce deployment innovations to prevent chronic disease. The Phase II survey findings provide indicators that LHDs may consider as they develop community assessments and plans for chronic disease prevention activities or prepare for the public health accreditation process.
Limitations
Although this study has many strengths, a few limitations must be noted. Most questions in Phase I were altered for Phase II, limiting our ability to compare data between time points. Altering the questions was deemed acceptable, however, because these surveys were not conceptualized to follow a pretest-posttest design. It is possible that the data aggregation methods (ie, decision rules) used to summarize multiple LHD responses into 1, for the purpose of the analysis, may have introduced a small amount of measurement error. On the other hand, incorporating multiple responses from some LHDs may have rendered the responses from those LHDs more accurate overall.
Conclusions
Prevention-focused funding, professional development activities, continued leadership from the public health field, and community engagement are needed to ensure that LHD gains in preventing obesity and chronic disease are leveraged and sustained and that conditions underlying chronic disease are addressed. The Phase II survey findings provide a benchmark from which further increases and improvements in chronic disease prevention practice in California LHDs may be measured.
Acknowledgments
This study was supported by a grant from The California Endowment. The authors acknowledge the contributions of Dr Heidi Skolnik, research analyst at The Sarah Samuels Center for Research and Evaluation. She analyzed the data and contributed to the synthesis and interpretation of the research findings.
Author Information
Corresponding Author: Liz Schwarte, MPH, Ad Lucem Consulting, 1339 Waller St, San Francisco, CA 94117. Telephone: 415-252-8646. E-mail: Liz@adlucemconsulting.com.
Author Affiliations: Samantha Ngo, MPH/MSW candidate at the University of California, Berkeley, Berkeley, California; Rajni Banthia, Resource Development Associates, Oakland, California; George Flores, The California Endowment, Oakland, California; Bob Prentice, Partnership for the Public’s Health/Public Health Institute, Oakland, California; Maria Boyle, Abt Associates, Inc, Cambridge, Massachusetts; Sarah E. Samuels, The Sarah Samuels Center for Public Health Research and Evaluation, Oakland, California. At the time of the study, Ms Schwarte, Ms Ngo, Dr Banthia, and Ms Boyle were affiliated with The Sarah Samuels Center for Public Health Research and Evaluation, Oakland, California. Dr Prentice is now retired. Sarah E. Samuels died March 29, 2014.
References
- Prentice B, Flores G. Local health departments and the challenge of chronic disease: lessons from California. Prev Chronic Dis 2007;4(1):A15. PubMed
- Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health 2010;100(4):590–5. CrossRef PubMed
- Summerbell CD, Waters E, Edmunds LD, Kelly S, Brown T, Campbell KJ. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2005;(3):CD001871. PubMed
- Lawrence S, Boyle M, Craypo L, Samuels S. The food and beverage vending environment in health care facilities participating in the Healthy Eating, Active Communities program. Pediatrics 2009;123(Suppl 5):S287–92. CrossRef PubMed
- Schwarte L, Samuels SE, Boyle M, Clark SE, Flores G, Prentice B. Local public health departments in California: changing nutrition and physical activity environments for obesity prevention. J Public Health Manag Pract 2010;16(2):E17–28. CrossRef PubMed
- Kuiper H, Jackson RJ, Barna S, Satariano WA. Local health department leadership strategies for healthy built environments. J Public Health Manag Pract 2012;18(2):E11–23. CrossRef PubMed
- Centers for Disease Control and Prevention. Vital signs: state-specific obesity prevalence among adults — United States, 2009. MMWR Morb Mortal Wkly Rep 2010;59(30):951–5. PubMed
- Williams E, Leachman M, Johnson N. State budget cuts in the new fiscal year are unnecessarily harmful: cuts are hitting hard at education, health care, and state economies. Washington (DC): Center on Budget and Policy Priorities; 2011.
- Institute of Medicine. Local government actions to prevent childhood obesity. Washington (DC): National Academy of Sciences; 2009.
- US Census Bureau. State and county quickfacts 2010. http://quickfacts.census.gov/qfd/states/06000.html. Accessed October 3, 2011.
- California Conference of Local Health Officers. Sacramento (CA): California Department of Public Health. http://www.cclho.org/. Accessed August 8, 2011.
- Bay Area Regional Health Inequities Initiative. Oakland (CA): Bay Area Regional Health Inequities Initiative. http://www.barhii.org/. Accessed January 15, 2013.
- Samuels S, Craypo L, Schwarte L, Yoshida S, Boyle M, Bullock S, et al. Healthy Eating, Active Communities and Central California Regional Obesity Prevention Program final evaluation synthesis report. Oakland (CA): Samuels and Associates; 2010.
- Case studies in chronic disease prevention: local health departments confront the challenge of the 21st century. Oakland (CA): Partnership for the Public’s Health, Public Health Institute; 2007.
- Samuels SE, Craypo L, Boyle M, Crawford PB, Yancey A, Flores G. The California Endowment’s Healthy Eating, Active Communities program: a midpoint review. Am J Public Health 2010;100(11):2114–23. CrossRef PubMed
- Schwarte L, Samuels SE, Capitman J, Ruwe M, Boyle M, Flores G. The Central California Regional Obesity Prevention Program: changing nutrition and physical activity environments in California’s heartland. Am J Public Health 2010;100(11):2124–8. CrossRef PubMed
- The California Health in All Policies Task Force. The Strategic Growth Council. http://sgc.ca.gov/s_hiap.php. Accessed September 22, 2014.
- Local public health department job losses and program cuts: findings from January 2011 survey and 2010 national profile study. Washington (DC): National Association of County and City Health Officials; 2011.
- Shortchanging America’s health: a state-by-state look at how federal public health dollars are spent and key state health facts. Washington (DC): Trust for America's Health; 2009.
- Prentice B, Galvez S. Local public health departments and chronic disease prevention: strategies for the recession and beyond. Oakland (CA): Partnership for the Public’s Health, Public Health Institute; 2011.
- Communities Putting Prevention to Work (CPPW). Atlanta (GA): Centers for Disease Control and Prevention; 2011. http://www.cdc.gov/healthycommunitiesprogram/communities/cppw/. Accessed November 30, 2011.
- Centers for Disease Control and Prevention. Community Transformation Grants. http://www.cdc.gov/nccdphp/dch/programs/communitytransformation/. Accessed September 22, 2014.
- Strategies for building community-public health partnerships: lessons learned from the program office of the Partnership for the Public’s Health initiative. Oakland (CA): Partnership for the Public’s Health Public Health Institute; 2007.
- CCLHO-CHEAC Chronic Disease Prevention Leadership Project. Chronic Disease Prevention Framework. Sacramento (CA): California Conference of Local Health Officers (CCLHO); 2013.
- Prevention and Public Health Fund. The Affordable Care Act. Washington (DC): US Department of Health and Human Services. http://www.hhs.gov/open/recordsandreports/prevention/. Accessed September 22, 2014.
Tables
 Table 1. Contributions to Increased Emphasis on Obesity and Chronic Disease Prevention by California Local Public Health Departmentsa (n = 39), 2006–2010
Table 1. Contributions to Increased Emphasis on Obesity and Chronic Disease Prevention by California Local Public Health Departmentsa (n = 39), 2006–2010
| Contributor | No. (%) Local Health Departments |
|---|---|
| Momentum in the field of obesity prevention | 30 (77) |
| Regional and state obesity and chronic disease prevention efforts | 26 (67) |
| Learning from other public health departments | 23 (59) |
| The California Endowment’s obesity and chronic disease prevention initiatives (eg, HEAC, CCROPP, Mini-grant) | 18 (46) |
| Local and state legislation supporting obesity and chronic disease prevention | 15 (39) |
| Technical assistance to public health departments | 15 (39) |
| Participation in other philanthropic initiatives (eg, HEAL, RWJF, other initiative) | 14 (36) |
| Leadership development programs or opportunities | 10 (26) |
Abbreviations: HEAC, Healthy Eating, Active Communities; CCROPP, Central California Regional Obesity Prevention Program; HEAL, Healthy Eating Active Living; RWJF, Robert Wood Johnson Foundation.
a Remaining local health departments surveyed either had not changed internally (n = 11) or did not know whether they had changed (n = 3).
 Table 2. Funding Sources for Obesity and Chronic Disease Prevention Activities in California Local Public Health Departments (LHDs) (N = 53), 2010
Table 2. Funding Sources for Obesity and Chronic Disease Prevention Activities in California Local Public Health Departments (LHDs) (N = 53), 2010
| Funding Source | No. (%) of LHDs With the Funding Source |
|---|---|
| Governmental funding | |
| Federal | 46 (87) |
| WIC | 35 (66) |
| Title V (MCAH) | 30 (57) |
| Title XIX (MCAH) | 18 (34) |
| ARRA | 8 (15) |
| Federal Transportation Funding SAFETEA-LU | 8 (15) |
| CDC Categorical funding | 3 (6) |
| CDC Steps to a Healthier US | 1 (2) |
| State | 43 (81) |
| Realignmenta | 32 (60) |
| California Department of Public Health Network for a Healthy California | 24 (45) |
| California Project LEAN | 5 (9) |
| California Active Communities Center for Physical Activity | 1 (2) |
| Local general fund | 26 (49) |
| Foundation funding | |
| One or more foundation funding sources | 26 (49) |
| Kaiser Permanente HEAL | 9 (17) |
| Kaiser Community Health Initiative | 9 (17) |
| HEAC | 7 (13) |
| CCROPP | 6 (11) |
| Healthy Kids Healthy Communities (RWJF) | 3 (6) |
| Active Living by Design (RWJF) | 2 (4) |
| Other foundation funding | 17 (32) |
Abbreviations: WIC, Special Supplemental Nutrition Program for Women, Infants, and Children; MCAH, Maternal, Child and Adolescent Health; ARRA, American Recovery and Reinvestment Act; SAFETEA-LU, Safe, Accountable, Flexible, Efficient Transportation Equity Act: a Legacy for Users; CDC, Centers for Disease Control and Prevention; LEAN, Leaders Encouraging Activity and Nutrition; HEAL, Healthy Eating Active Living; HEAC, Healthy Eating, Active Communities; CCROPP, Central California Regional Obesity Prevention Program; RWJF, Robert Wood Johnson Foundation.
a In California, “realignment” refers to funding from the transfer of program responsibility and revenue sources for sales tax and vehicle license fees from the state to counties.
 Table 3. California Local Public Health Departments’ (LHDs’) Engagement in Obesity and Chronic Disease Prevention Activities, 2010
Table 3. California Local Public Health Departments’ (LHDs’) Engagement in Obesity and Chronic Disease Prevention Activities, 2010
| Activity | No. (%) of All LHDs (N = 53) | No. (%) of LHDs with Foundation Funding (n = 26) | No. (%) of LHDs Without Foundation Funding (n = 27) | No. (%) of LHDs With a Person or Unit Leading Obesity and Chronic Disease Prevention Efforts (n = 38) |
|---|---|---|---|---|
| Research and data | ||||
| Monitor obesity health indicators (eg, BMI, California Health Interview Survey) | 47 (89) | 24 (92) | 23 (85) | 35 (92) |
| Morbidity and mortality data linked to health equity efforts | 34 (64) | 19 (73) | 15 (56) | 27 (71) |
| Built environment assessments (eg, walkability assessments) | 30 (57) | 21 (81) | 9 (33) | 29 (76) |
| GIS mapping | 27 (51) | 17 (65) | 10 (37) | 24 (63) |
| CX3 assessments | 25 (47) | 19 (73) | 6 (22) | 23 (61) |
| Health impact assessments | 14 (26) | 12 (46) | 2 (7) | 12 (32) |
| Collaboration | ||||
| Participate in school or community obesity prevention collaboratives | 46 (87) | 24 (92) | 22 (82) | 34 (90) |
| Participate in city, county, or regional planning commissions or committees focused on improving built environment | 44 (83) | 25 (96) | 19 (70) | 35 (92) |
| Facilitate farmers market, agricultural industry, or food security program collaboration to increase access to healthful food | 38 (72) | 22 (85) | 16 (59) | 32 (84) |
| Participation with other public health departments in regional obesity prevention | 32 (60) | 22 (85) | 10 (37) | 26 (68) |
| School health | ||||
| Improve beverage and/or food environment | 32 (60) | 19 (73) | 13 (48) | 29 (76) |
| Ensure quality PE or physical activity opportunities (eg, enforce state PE requirements) | 22 (42) | 13 (50) | 9 (33) | 19 (50) |
| Ensure free, safe drinking water availability | 16 (30) | 11 (42) | 5 (19) | 15 (40) |
| Food retail | ||||
| Enable small store owners to carry more healthful, affordable food items | 22 (42) | 18 (69) | 4 (15) | 22 (58) |
| Support incentive programs or use zoning laws to attract supermarkets and grocery stores to underserved neighborhoods | 16 (30) | 11 (42) | 5 (19) | 16 (42) |
| Limit fast food restaurant access through policy or zoning measures | 12 (23) | 9 (35) | 3 (11) | 12 (32) |
| Community food access | ||||
| Encourage farmers markets to accept federal food program benefits (eg, WIC) | 38 (72) | 24 (92) | 14 (52) | 31 (82) |
| Encourage farmers markets and/or produce stand establishments | 35 (66) | 22 (85) | 13 (48) | 31 (82) |
| Monitor chain restaurant menu labeling and/or encourage nonchain restaurants to provide calorie information | 15 (28) | 12 (46) | 3 (11) | 14 (37) |
| Offer incentives (eg, recognition) to restaurants that promote more healthful options | 7 (13) | 7 (27) | 0 | 7 (18) |
| Public and worksite programs | ||||
| Support worksite nutrition standards and/or physical activity guideline development and implementation | 22 (42) | 19 (73) | 3 (11) | 22 (58) |
| Support public venue nutrition standards and/or physical activity guideline development and implementation | 22 (42) | 15 (58) | 7 (26) | 21 (55) |
| Physical activity environments | ||||
| Support sidewalk and street crossing planning, and building to encourage walking | 36 (68) | 23 (89) | 13 (48) | 33 (87) |
| Develop and implement Safe Routes to School programs with schools to increase walkability and bikability | 32 (60) | 22 (85) | 10 (37) | 29 (76) |
| Support safe and attractive park and playground development near residential areas | 28 (53) | 16 (62) | 12 (44) | 25 (66) |
| Establish joint use of facilities agreements between school districts and other organizations | 26 (49) | 18 (69) | 8 (30) | 24 (63) |
| Other policies or ordinances | ||||
| Promote air quality improvements, including greenhouse gas reduction, transportation redesign | 20 (38) | 17 (65) | 3 (11) | 19 (50) |
| Promote tax or fee to discourage nutrient-poor foods and beverages | 16 (30) | 12 (46) | 4 (15) | 14 (37) |
| Inform federal food legislation (eg, Child Nutrition Reauthorization Act) | 15 (28) | 10 (39) | 5 (19) | 12 (32) |
| Develop local ordinances to restrict nutrient-poor mobile vending near schools and/or public playgrounds | 10 (19) | 8 (31) | 2 (7) | 9 (24) |
| Eliminate nutrient-poor food and beverage marketing in children’s environments | 7 (13) | 5 (19) | 2 (7) | 6 (16) |
Abbreviations: BMI, body mass index; GIS, geographic information systems; CX3, Communities of Excellence; PE, physical education; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions.