 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Assessment of Increase in Perinatal Exposure to HIV Among Hispanics --- 20 Counties, Georgia, 1994--2002CDC recently received reports from clinicians in a specialized pediatric human immunodeficiency virus (HIV) care clinic (clinic A) suggesting that the number of perinatally HIV-exposed Hispanic infants in the Atlanta metropolitan area had increased disproportionately to the growth of Hispanics in the area's population. To assess this increase and characterize trends in perinatal HIV exposure in this population, CDC collaborated with health-care providers at clinic A, which serves residents in 20 Georgia counties, including the Atlanta metropolitan area. This report summarizes the results of that assessment, which suggest that the increase in the number of perinatally HIV-exposed Hispanic infants was associated with multiple factors, including the growth of the Hispanic population, increasing HIV prevalence and fertility among Hispanics, and lower preconception awareness of HIV serostatus among those with HIV. The findings suggest a need for improved access to voluntary HIV counseling and testing and increased opportunities for reducing the risk for unintended pregnancy among Hispanics in these counties. Data on maternal race/ethnicity and infant final HIV-infection status were obtained from Ryan White Comprehensive AIDS Resource Emergency records maintained by clinic A. Infants born during 1994--2002 were referred to the clinic because 1) HIV infection had been diagnosed in the mother preconception, and the infant had perinatal exposure to HIV or 2) the infant was believed to have acquired perinatal HIV infection from the mother. In this report, Hispanics might be of any race; non-Hispanics were classified either as non-Hispanic black or as "non-Hispanic white and other races." The HIV-infection rate for each racial/ethnic population was defined as the number of infants who were HIV infected divided by the total number of infants who were exposed perinatally. During the study period, HIV infection (i.e., without acquired immunodeficiency syndrome [AIDS]) was not reportable in Georgia. Thus, the number of women with HIV infection giving birth in Georgia and the proportion of perinatally HIV-exposed or perinatally HIV-infected infants in the 20 counties who did not receive care from clinic A is unknown. However, approximately 70% of Georgia AIDS cases were reported from five metropolitan Atlanta counties (1), and clinic A is the state's principal provider of specialized pediatric HIV health care. The numbers of live births by year and maternal race/ethnicity were obtained by using the Online Analytical Statistical Information System (OASIS) of the Georgia State Division of Public Health (2). U.S. Census data for 2001 were used to estimate racial/ethnic trends in the female populations of childbearing age in those counties (3). Data from HIV serologic surveys of childbearing women, which are no longer conducted in the United States, can be compared with other health data to describe the dynamic of HIV among women of childbearing age (4). As an alternative to a serologic survey of childbearing women, minimum HIV seroprevalence among women who gave birth in 2002 and among all women who were of childbearing age in the 20 Georgia counties was estimated by using the number of infants known to be perinatally HIV exposed in 2002 as the numerator. The numbers of women of childbearing age and of women who delivered live infants in these counties in 2002 were used as the denominators (2,3). During 1994--2002, the number and proportion of live births to Hispanics in the 20 counties increased more than threefold, from 5.0% (2,620) to 16.8% (11,130) (1) (Figure). Conversely, during the same period, although the number of live births increased, the proportion of births to non-Hispanic whites and other races declined from 60.5% (31,612) to 50.3% (33,256), and the proportion to non-Hispanic blacks declined from 34.5% (18,017) to 32.9% (21,765). The estimated proportion of Hispanics in Georgia's population of females of childbearing age increased from 2.5% to 6.1% during this same period (3). The proportion of perinatally HIV-exposed infants who were Hispanic increased by more than ninefold, from one of 96 (1.1%) in 1994 to 10 of 95 (10.5%) in 2002 (p<0.001) (Table). Among HIV-exposed infants who were non-Hispanic white and other races, the proportion increased from five of 96 (5.2%) in 1994 to seven of 95 (7.4%) in 2002; among infants who were non-Hispanic black, the proportion decreased from 90 (94.0%) of 96 in 1994 to 78 (82.0%) of 95 in 2002. The proportion of HIV seroprevalence to live births among childbearing women in the 20 counties in 2002 was estimated at 0.36% (78 HIV-exposed infants of 21,765 live births) among non-Hispanic blacks, 0.09% (10 HIV-exposed infants of 11,130 live births) among Hispanics, and 0.02% (seven HIV-exposed infants of 33,256 live births) among non-Hispanic whites and other races (p<0.01). Assuming that HIV seroprevalence among women of childbearing age in these counties was similar to that among women who gave birth to a live infant in 2002, 0.36% of 341,379 non-Hispanic blacks (1,229), 0.09% of 79,237 Hispanics (71), and 0.02% of 620,743 non-Hispanic whites and other races (124) had HIV infection. On the basis of these estimates, 10 (14.1%) of 71 HIV-infected Hispanic women had a live birth in 2002, compared with 78 (6.3%) of 1,229 non-Hispanic black women and seven (5.6%) of 124 women of non-Hispanic white and other races (Fisher's exact 2-tailed p<0.03). In contrast to the proportion of Hispanic women living with HIV who gave birth in 2002, only 2.5% of women receiving services at clinic A were Hispanic. Reported by: S Nesheim, MD, R Dennis, V Grimes, Emory Univ School of Medicine, Atlanta; RL Shouse, MD, Georgia State Div of Public Health. K Dominguez, MD, Div of HIV/AIDS Prevention, National Center for HIV, STD, and TB Prevention; Z Ali, CM Beck-Sague, MD, Div of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion; K Asamoa, MD, EIS Officer, CDC. Editorial Note:Although the increase in number and proportion of perinatally HIV-exposed Hispanic infants outpaced the increase in the proportion of births that occurred among Hispanics in Georgia and Atlanta (2), the findings in this report suggest that the increase in perinatal HIV-exposure in 20 Georgia counties in part was associated with increased fertility rate. During the preceding 20 years, the U.S. Hispanic population approximately doubled because of an unprecedented level of immigration and the highest fertility rate of any U.S population group (3,5). The growth in the number of Hispanics was particularly large in metropolitan areas in the U.S. Southeast, where Atlanta had the greatest increase. In 2002, among all U.S. regions, the Southeast had the largest estimated number of persons living with HIV/AIDS (6). Although Hispanics do not represent a large percentage of persons with AIDS in Georgia, they have experienced the largest increases in AIDS cases (1). Nationwide, compared with other population groups, Hispanics with HIV infection are substantially less likely to have had two or more outpatient visits during the preceding 6 months, more likely to have HIV infection diagnosed late in the course of their disease, and less likely to have health insurance (7). The small proportion of Hispanic female patients at clinic A in 2002 suggests that these national trends also might have occurred among HIV-infected Hispanics in Atlanta. In the 1995 National Survey of Family Growth, Hispanic women were less likely than those other U.S. population groups to use contraception during their first intercourse or to use reversible contraception (8). In the 20 Georgia counties studied in this report, 16% of Hispanic women of childbearing age had a live birth in 2002, compared with 6.3% of non-Hispanic black women and 5.4% of women who were non-Hispanic white and other races (2). Less use of health resources (e.g., HIV testing and family planning services) by Hispanic women in these counties might contribute to their overrepresentation among childbearing women with HIV. The findings in this report are subject to at least four limitations. First, the small number of perinatally HIV-exposed Hispanic infants limits the precision of estimates. Second, identification bias might have reduced the number of mothers classified as Hispanic in 1994, exaggerating the increase in the Hispanic proportion of perinatally HIV-exposed infants. Third, because perinatally HIV-exposed infants were identified through voluntary counseling and testing of mothers, certain mothers whose status was not determined might have been HIV infected but not included. Finally, although national estimates and international comparisons of HIV seroprevalence continue to be based on sentinel surveillance among pregnant women, HIV seroprevalence among childbearing women might not be similar to that in the general population. Because HIV infection reduces fertility, particularly later in the course of HIV infection, the seroprevalence in childbearing women might underestimate seroprevalence among other women (9). All sexually active women of childbearing age, particularly those in areas with high HIV/AIDS prevalence, should be advised of the potential for remaining symptom-free if HIV infection is diagnosed and treated before the onset of severe immunodeficiency (10). Opportunities for HIV testing, ideally before conception, but also during pregnancy, should be increased. HIV testing during labor should be considered a community standard of care for women who have not been tested during pregnancy. In addition, linkages should be offered to specialized treatment and prevention services, including family planning services, for all women who wish to delay childbearing to reduce the risk for both sexual and perinatal HIV transmission and to improve symptom-free survival among underserved women living with HIV. References
Table 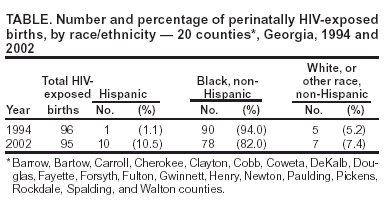 Return to top. Figure 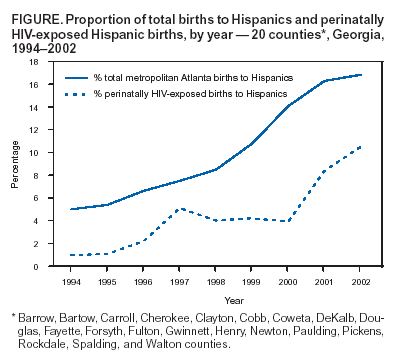 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 10/14/2004 |
|||||||||
This page last reviewed 10/14/2004
|