Key points
- Measles is a highly contagious respiratory virus that causes febrile rash illness.
- Recognize the common signs of measles and the course of disease.
- Learn what to do if you have a suspected case of measles.
Text equivalent
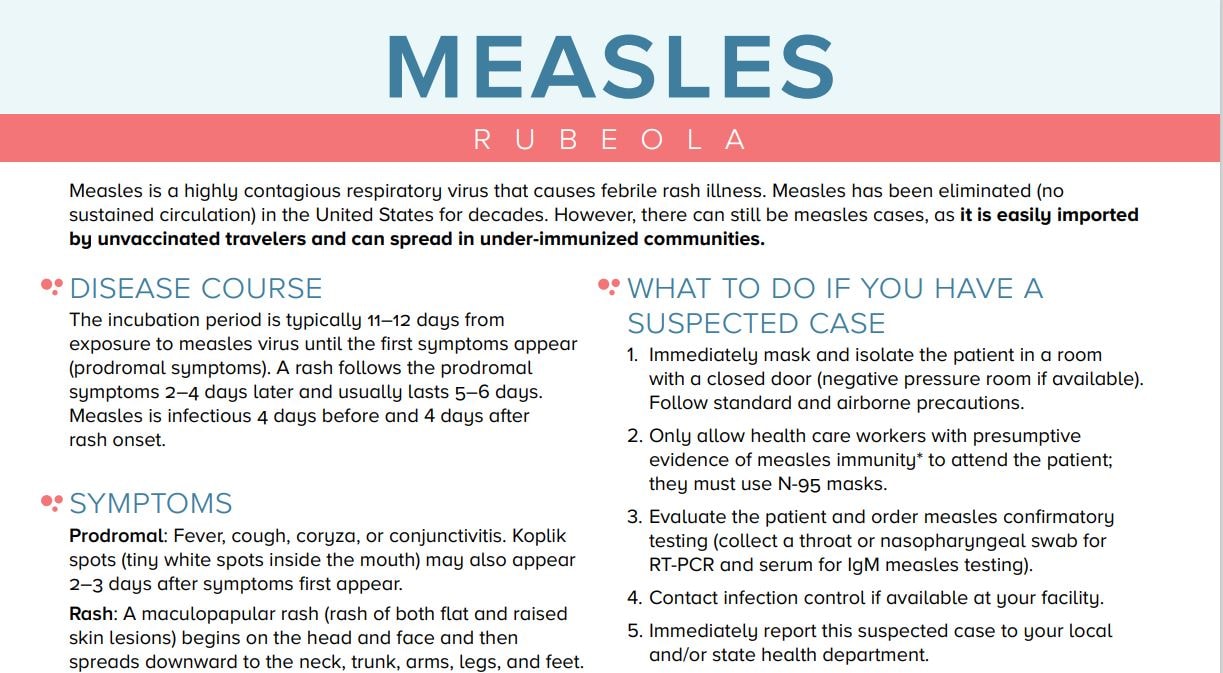
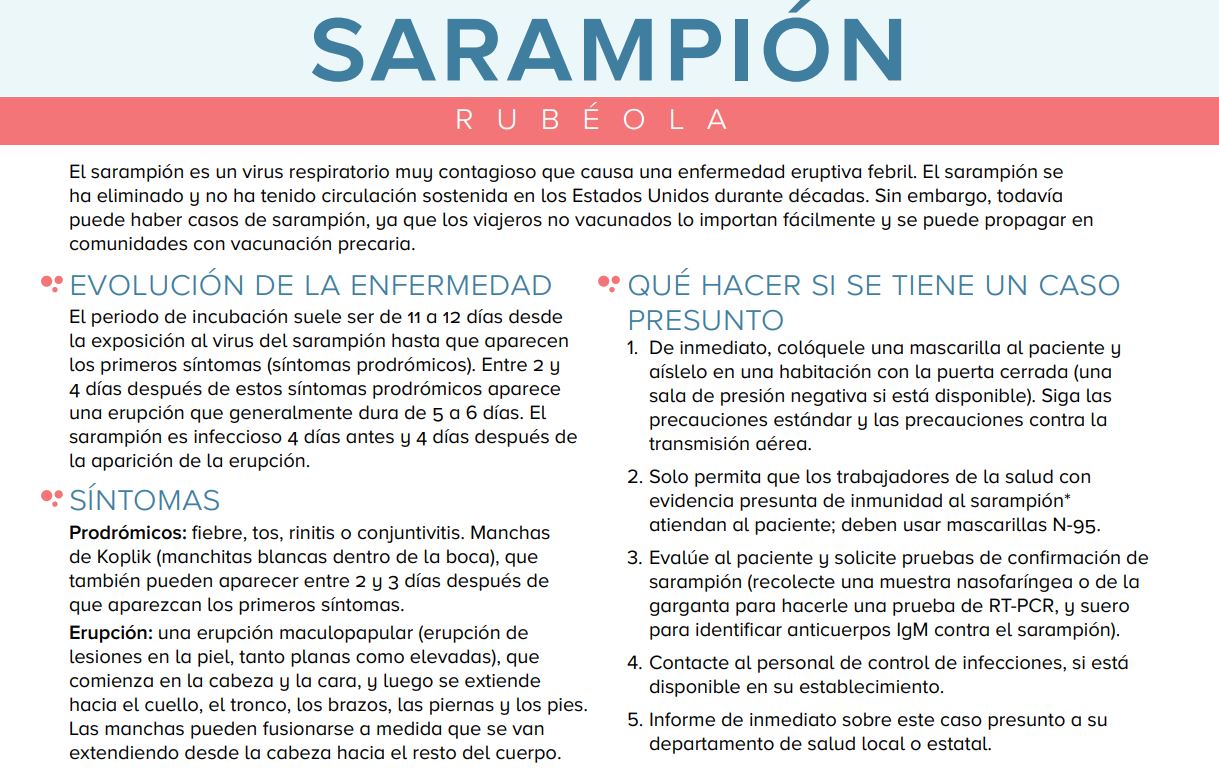
Measles (Rubeola)
Measles is a highly contagious respiratory virus that causes febrile rash illness. Measles has been eliminated (no sustained circulation) in the United States for decades. However, there can still be measles cases, as it is easily imported by unvaccinated travelers and can spread in under-immunized communities.
Disease course
The incubation period is typically 11–12 days from exposure to measles virus until the first symptoms appear (prodromal symptoms). A rash follows the prodromal symptoms 2–4 days later and usually lasts 5–6 days. Measles is infectious 4 days before and 4 days after rash onset.
Symptoms
Prodromal: Fever, cough, coryza, or conjunctivitis. Koplik spots (tiny white spots inside the mouth) may also appear 2–3 days after symptoms first appear.
Rash: A maculopapular rash (rash of both flat and raised skin lesions) begins on the head and face and then spreads downward to the neck, trunk, arms, legs, and feet. The spots may become joined together as they spread from the head to the body. Fever may spike to more than 104° F when rash appears.
Complications
Most common complications: Diarrhea and otitis media.
Most severe complications: Pneumonia, encephalitis, and death. Patients may require hospitalization. Children younger than 5, adults older than 20, pregnant women, and immunocompromised persons are at most risk of serious complications.
What to do if you have a suspected case
- Immediately mask and isolate the patient in a room with a closed door (negative pressure room if available). Follow standard and airborne precautions.
- Only allow health care workers with presumptive evidence of measles immunity* to attend the patient; they must use N-95 masks.
- Evaluate the patient and order measles confirmatory testing (collect a throat or nasopharyngeal swab for RT-PCR and serum for IgM measles testing).
- Contact infection control if available at your facility.
- Immediately report this suspected case to your local and/or state health department.
For questions regarding specimen collection, storage, and shipment, please visit https://www.cdc.gov/measles/lab-tools/rt-pcr.html
*Presumptive evidence of measles immunity for healthcare workers (one of the following): documentation of two doses of measles-containing vaccine, laboratory evidence of immunity (positive IgG), laboratory evidence of disease, or birth before 1957. Consider vaccinating healthcare workers born before 1957 who do not have other evidence of immunity to measles. Self-reported doses and a history of vaccination provided by a parent or other caregiver, or a clinical diagnosis of measles, should not be accepted.
Resources
- Measles information for healthcare providers: https://www.cdc.gov/measles/php/laboratories/
- Measles vaccine recommendations: https://www.cdc.gov/measles/hcp/vaccine-considerations/
- Infection control guidelines for measles: https://www.cdc.gov/infection-control/hcp/measles/
- Surveillance manual chapter on measles: https://www.cdc.gov/vaccines/pubs/surv-manual/chpt07-measles.html
[Image of measles on the face]
[Image of measles on the trunk of body]
08/02/24
Centers for Disease Control and Prevention
National Center for Immunizationand Respiratory Diseases