What to know
ME/CFS is a chronic, multisystem illness. People with ME/CFS are often unable to do their previous activities. Some people may be homebound or even bedbound. About 9 in 10 people with ME/CFS have not been diagnosed. ME/CFS often follows an infection. Other triggers include trauma, stress, and toxins.

What it is
ME/CFS is a disabling and complex illness. The cause of ME/CFS is unknown, and there is no specific test to diagnose ME/CFS. Instead, healthcare providers can use diagnostic criteria developed in 2015 by the Institute of Medicine (IOM).
The patient must have all three of the following symptoms:
- Decreased activity levels for more than 6 months, with new fatigue not relieved by rest.
- Post-exertional malaise.
- Unrefreshing sleep.
And at least one of two of the following symptoms:
- Problems thinking or concentrating.
- Dizziness or fainting when standing (known as orthostatic intolerance).
When diagnosing ME/CFS, it is important to assess the frequency and severity of symptoms.
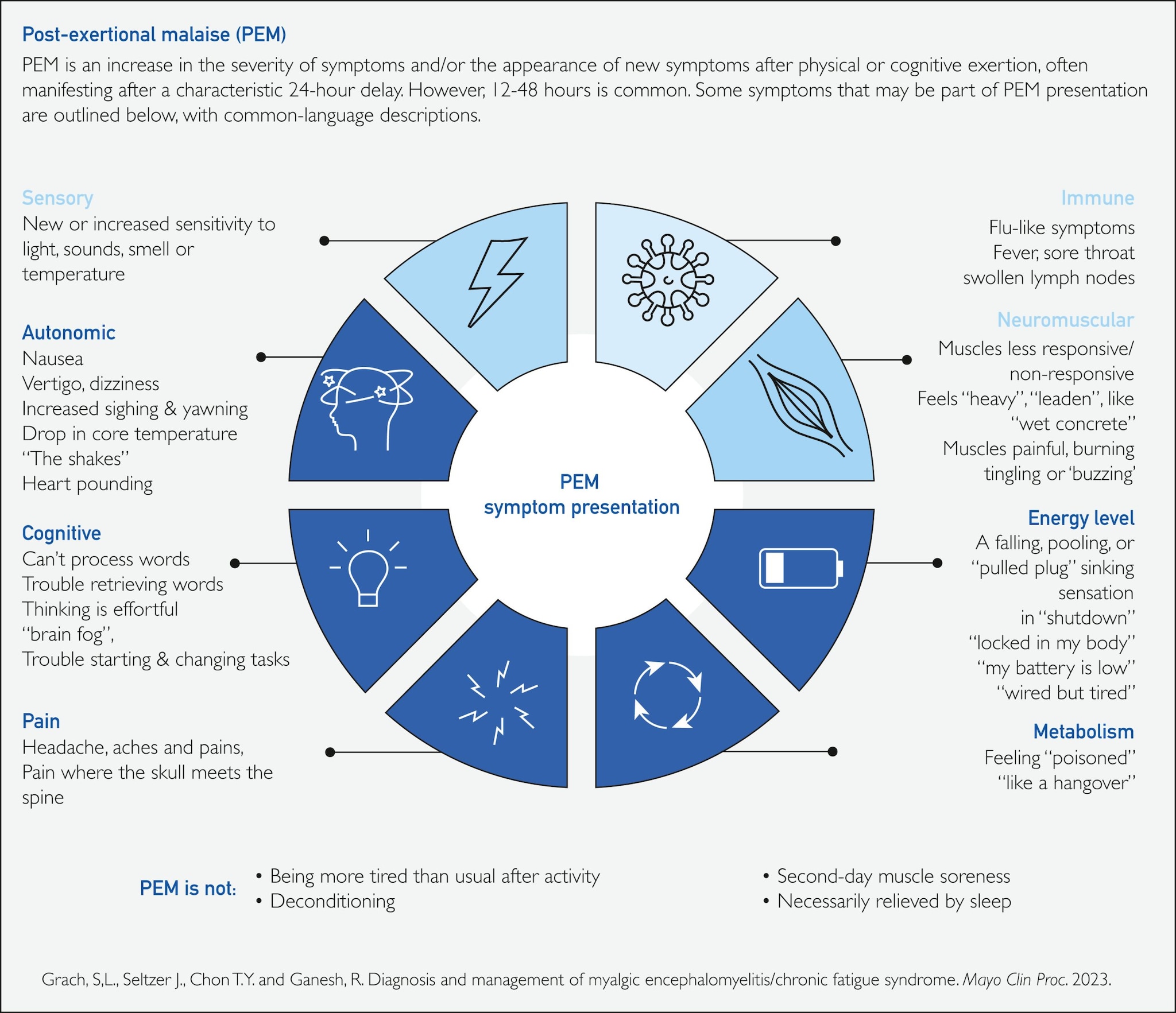
What is Post-Exertional Malaise (PEM)?
PEM is worsening of ME/CFS symptoms after physical or mental activity that wouldn't have caused problems previously. During PEM, ME/CFS symptoms may get worse or appear for the first time.
Symptoms may include:
- Difficulty thinking
- Problems sleeping
- Headaches
- Feeling dizzy
- Severe tiredness
It may take days, weeks, or longer to recover from PEM. People with ME/CFS often describe this experience as a "crash," "relapse," or "collapse."
Who's affected
Anyone can get ME/CFS.
- In adults, ME/CFS affects more women than men.
- People who are Black and Latino may be more affected.
- ME/CFS is most common in people between the ages of 40-60 years.
- ME/CFS is more common in adolescents than young children.
- People of all income levels can get ME/CFS.
- Between 836,000 to 3.3 million people in U.S. have ME/CFS.
Treatment
There is no cure for ME/CFS, but symptoms can be treated or managed. ME/CFS treatment plans should include input from each patient. The benefits and harms of medications or other therapies should be discussed.
Symptoms that cause the most problems should be treated first. Learning ways to manage activity may be helpful.
Frequently asked questions
Where can I find a healthcare provider for ME/CFS?
CDC does not provide a list of healthcare providers for diseases or illness. A healthcare provider who listens and works with patients can make a diagnosis of ME/CFS. More information can also be found at Patient and Caregiver Resources - Solve ME/CFS Initiative (solvecfs.org).
What tests are there for ME/CFS?
There is not a specific test to diagnose ME/CFS. A healthcare provider can make a diagnosis using the 2015 IOM Case Definition.
Is ME/CFS a real illness?
ME/CFS is a real, legitimate illness. It affects multiple body systems. It needs to be diagnosed and treated.
What's it like to live with ME/CFS?
ME/CFS affects each person differently. To hear more about ME/CFS from patients with the illness, please visit Living with ME/CFS page.
