Key points
- Legionellosis, which includes Legionnaires' disease, is a nationally notifiable disease.
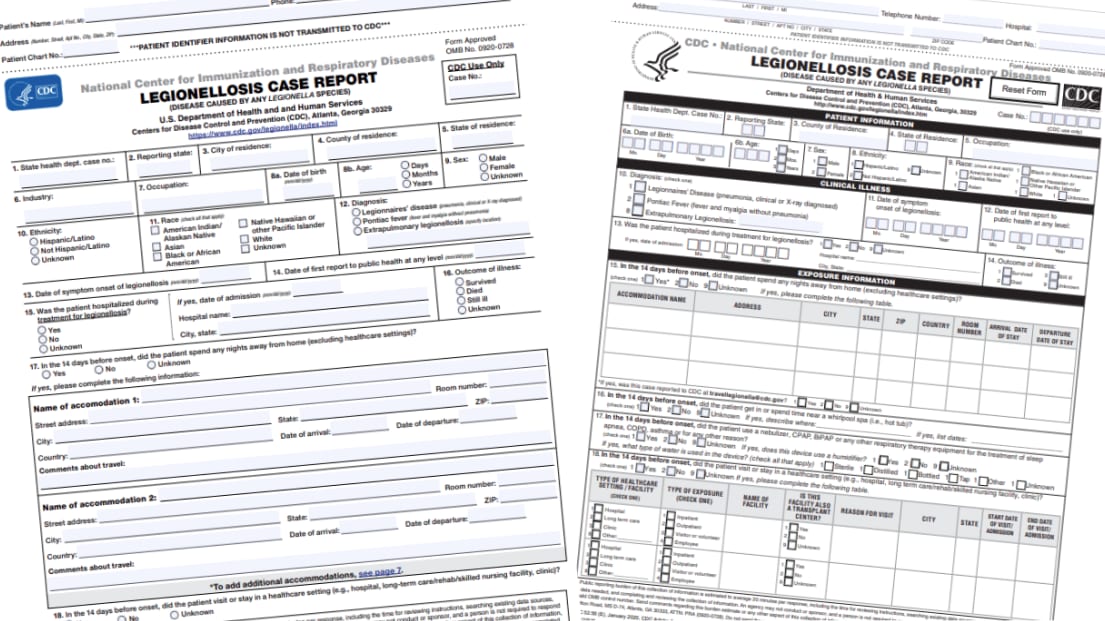
- Report cases to the Supplemental Legionnaires' Disease Surveillance System (SLDSS) using any of the following forms.
Data reporting
After choosing the form you want to use, complete as much of it as possible. Travel-related reports should include
- Travel destination(s)
- Accommodation or facility name[s] and address[es]
- Dates of travel
- Notable water exposures during travel
If you have questions, email travellegionella@cdc.gov.
Extended case report form
A form with additional variables (beyond those on the Core Form) for jurisdictions able to collect expanded exposure or comorbidity information. Additional variables are consistent with the Legionellosis Message Mapping Guide. This form can also be used for hypothesis generation during case investigations.
- Extended Form last updated 02/02/2023
- Spanish Version last updated 02/02/2023
Core case report form
A shorter form with SLDSS core variables.
- Core Form last updated 01/23/2020
Cruise exposure reporting
For cases with cruise travel during the exposure period, complete the cruise ship questionnaire template. Submit the completed questionnaire when reporting travel-associated cases.
Submitting forms to CDC
Mail: Centers for Disease Control & Prevention
ATTN: Respiratory Diseases Branch
Mailstop H24-8
1600 Clifton Rd NE
Atlanta, GA 30329-4027
Fax: (404) 315-4680
Email: travellegionella@cdc.gov
SLDSS reporting timelines
Any case: Ideally within 30 days of receiving a case report
Travel-associated cases: Within 7 days of receiving a case report
CDC also accepts bulk case data in Excel or CSV files using a standardized format. This is the preferred submission method, although travel reports should be submitted within 7 days via email or fax. Email us for more information about bulk data extract submissions.
Instructions for completing the forms
Extended form
The new Extended Form includes all the variables found in the Core Form. It also includes variables to assist in the hypothesis-generating process. Two new sections obtain information on the case patient's expanded exposures and underlying conditions. Download the Extended Case Report Form.
Instructions are currently under development for the Extended Form.
Core form
The Core Form contains the core variables necessary to report legionellosis cases to SLDSS. Jurisdictions should continue to complete the Core Form if resources don't allow for the completion of the Extended Form. Download the Core Case Report Form.
Use the instructions below in conjunction with the CDC Legionellosis Case Report Core Form.
Section 1. Patient Information and Demographics
State health dept. case no.: Enter the unique identifier assigned by the state health department.
Reporting state: Use the 2 letter postal abbreviation (e.g., GA) of the state health department reporting to CDC.
County of residence: Indicate the patient’s county of residence.
State of residence: Use the 2 letter postal abbreviation (e.g., GA) of patient’s state of residence.
Occupation: Indicate occupation of patient at time of symptom onset. Please consider occupational settings that may expose the patient to aerosolized water, such as maintenance (e.g., water service provider, water appliances, cooling towers), construction, leisure (e.g., hotel, cruise ship, water park), industrial/manufacturing plants with water spray systems, and long-haul/commercial truck drivers.
Date of birth: Enter date of birth of patient in this format (mm/dd/yyyy).
Age: Enter age of patient at time of symptom onset; indicate age unit as days, months, or years.
Sex: Indicate sex of patient.
Ethnicity: Indicate ethnicity of patient.
Race: Indicate race of patient, using multiple boxes if needed. Do not make assumptions based on name or native language. If race is unknown, please check “Unknown.”
Section 2. Clinical Information and Outcome
Diagnosis: Indicate legionellosis type:
- Legionnaires’ disease
- Pontiac fever
- Extrapulmonary legionellosis
- Although extremely rare, Legionella can also cause extrapulmonary infections, such as endocarditis or wound infections.
- If you select Extrapulmonary legionellosis please specify anatomic location of infection.
- Extrapulmonary legionellosis is not intended to reflect “unknown.” Please make your best attempt to categorize cases in one of these three discrete categories.
Refer to CDC’s Clinical Features page for key clinical differences between Legionnaires’ disease and Pontiac fever. Learn more about the CSTE case definition. Additional criteria for defining Legionnaires’ disease and Pontiac fever are subject to local health department jurisdictions. CDC is available for consultation and assistance for questions.
Date of symptom onset: Enter the date (mm/dd/yyyy) when patient-described signs and symptoms of legionellosis first occurred. If the patient had existing respiratory symptoms at baseline (e.g., chronic cough), use the date when symptoms got worse. If exact date is unavailable, enter the best guess based on medical records and patient/proxy interviews. Use the Comments field for any discrepancies (e.g., between patient/proxy interviews and medical records), or if date is unsure.
Date of first report to public health at any level: Enter date (mm/dd/yyyy) when this case was first reported to public health at any level of jurisdiction.
Hospitalization: Indicate whether the patient was hospitalized during treatment for legionellosis. If so, enter the admission date (mm/dd/yyyy), full name of hospital (without acronyms or abbreviations), and the city and state of the hospital. If the patient was admitted to a hospital before the date of legionellosis symptom onset and/or admitted due to non-legionellosis reasons, please enter the hospitalization information in the healthcare exposure section (Q18 and Q19).
Outcome: Indicate if the patient survived, died, or is still ill from this illness at time of reporting. If unknown, indicate “Unknown.”
Section 3. Travel, Healthcare, and Other Exposure Information
Travel: Indicate whether the patient spent any nights away from home, whether in-state, out-of-state, or out of the country, in the 14 days before onset excluding healthcare settings and senior/assisted living facilities. If travel was to a healthcare setting or a senior/assisted living facility, please enter this information in Q18, Q19 and Q20, respectively. For this section, please include:
- Complete name of hotel or travel accommodation
- Full address, city, state, zip code, and country
- Dates of arrival and departure
- The room number (or floor level), if known
As travel can occur in various settings, refer to the table below for examples on the types of travel information captured by our surveillance system:
| Types of travel | Examples | Additional guidance |
|---|---|---|
| Private | Homes of family and friends, mobile homes, motor homes, trailers | Include the address to the best of your ability and indicate that travel was at a private residence. |
| Public | Hotels and resorts, vacation/home rentals (such as Airbnb.com and VRBO.com), RV parks and resorts, state parks, campgrounds, truck stops | Include the name and address of the public accommodation. |
| Cruise | River and ocean cruises | Enter cruise line and ship name, departure port location (city, state), departure and return dates, and cabin number. |
Additionally, patients may stay overnight at congregate living facilities, such as shelters or correctional facilities. Although CDC does not consider this type of setting to be travel-associated according to the surveillance definition, it is still important to systematically capture these settings as part of the patient’s exposure history. The best place to enter this information would be in this section. You can enter additional details in the Comments field as needed.
Hot tub exposure: Indicate whether the patient spent time near or inside a hot tub with water jets (e.g., Jacuzzi®, whirlpool spa, hydrotherapy tub) in the 14 days before onset. Hot tub exposure can occur in a variety of settings, such as healthcare facilities, fitness centers/gyms, hotels/resorts, fairs, home and garden shows with hot tub displays, cruises, vacation rental units/homes, and community complexes. If so, indicate the location name and dates of exposure.
Respiratory therapy equipment usage: Indicate whether the patient has used a nebulizer, CPAP, BiPAP, or any other respiratory therapy equipment (for treatment of sleep apnea, COPD, asthma, or for any other reason) in the 14 days before symptom onset. If yes, indicate if the device uses a humidifier. If the device uses a humidifier, indicate the type of water that it uses (check all that apply).
Healthcare setting: Indicate whether the patient spent any time in a healthcare setting in the 14 days before onset. CDC defines a healthcare setting/facility as a hospital, long-term care facility, or clinic. Refer to the table below for healthcare facility categories and examples of facilities that fall within them.
| Hospitals | Long-term care facilities | Clinics1 |
|---|---|---|
|
|
1 Examples of specialty clinics include outpatient cancer treatment centers, outpatient infusion centers, dental offices, or subspecialist offices that provide clinical care not affiliated with a hospital. Other healthcare facilities not listed here include associated sites such as pharmacies and outpatient laboratories.
2 If a clinic visit or same-day surgery occurs within a hospital, the setting for that exposure is hospital, not clinic.
Type of healthcare exposure: Indicate the type of healthcare exposure, which is defined as inpatient, outpatient, visitor/volunteer, or employee. For surveillance purposes, indicate “inpatient” if the patient spent any nights in the facility.
Healthcare facility details: Enter the complete name of the facility and building (without acronyms or abbreviations), if applicable, including city and state. Indicate whether this facility is also a transplant center. Include the reason and dates of visit. If the patient visits a facility X number of times throughout a time period, please indicate this information either in this section or in the Comments section.
Healthcare exposure determination: Further classify the healthcare exposure based on the duration of healthcare exposure:
- Presumptive healthcare-associated Legionnaires’ disease: A case with ≥10 days of continuous stay at a healthcare facility during the 14 days before onset of symptoms.
- Possible healthcare-associated Legionnaires’ disease: A case that spent a portion of the 14 days before date of symptom onset in one or more healthcare facilities, but does not meet the criteria for presumptive healthcare-associated Legionnaires’ disease.
Note the following:
- Visitor and employee visits to healthcare facilities during their exposure period are considered possible healthcare-associated.
- A patient who spent ≥10 days of continuous stay in multiple healthcare facilities would be considered a presumptive healthcare-associated case for surveillance purposes.
- If there are pertinent healthcare exposures outside of the 14 day exposure period, these can be noted in the Comments field even though this would not be considered a healthcare-associated case for surveillance purposes.
Refer to the table below for example scenarios and corresponding responses to Q18 and Q19:
| Scenario | Q18. In the 14 days before onset, did the patient visit or stay in a healthcare setting? | Q19. Case associated with healthcare exposure? |
|---|---|---|
| Did not visit in the 14 days before date of symptom onset | Indicate "No." | Indicate "No." |
| Visited more than 14 days before date of symptom onset | Indicate “No,” but details about that visit may still be recorded in this section. | Indicate "No." |
| Visited in the 14 days before date of symptom onset | Indicate “Yes.” This visit should be documented with start and end dates. If the patient visited the facility and left on the same day, please enter the date of visit for both “start date” and “end date,” to indicate that the patient did not stay overnight.
If the patient visits a facility X number of times, please indicate this information either in this section or in the Comments field. |
Indicate “Presumptive” or “Possibly,” depending on duration of exposure during exposure period. |
| Visited in the 14 days before date of symptom onset but exact dates are not known | Indicate “Yes.” If specific dates are unclear, leave start and/or end dates blank, but efforts should be made to verify the date(s). Consider contacting the facility if the patient is unsure of the dates.
If the patient has been a resident of a long-term care facility for a duration much longer than 14 days (e.g., months, years), the date of admission may not be known. If the facility cannot document the admission date, enter the year at a minimum. If the patient has been residing at the long-term care facility until he/she was hospitalized due to legionellosis, that date should be entered as the end date. |
Indicate “Presumptive” or “Possibly,” depending on duration of exposure during exposure period. |
| Unknown | Indicate "Unknown." | Indicate "Unknown." |
Assisted and senior living facility: Indicate the type of exposure, which is defined as resident, visitor/volunteer, or employee. Enter the complete name (without acronyms or abbreviations), city, and state of the facility, as well as dates of stay. Assisted living facilities provide custodial care and assistance with activities of daily living, such as bathing and dressing. Senior living facilities (including retirement homes without skilled nursing or personal care) provide independent living for the elderly. CDC does not consider assisted or senior living facilities to be healthcare facilities. Community-based residential facilities and other residential facilities that do not provide skilled nursing care are included in this section.
Outbreak: Indicate if this case is associated with a known outbreak or possible cluster. If yes, specify the associated establishment (if applicable), city, and state of the outbreak or cluster.
Section 4. Laboratory Data
Learn more about the CSTE case definition.
Confirmed Case
Urinary antigen positive: If the clinician performed a urinary antigen test and it was positive, enter the sample collection date.
Culture positive: If there was a positive culture of any Legionella organism from respiratory secretions, lung tissue, pleural fluid, or extrapulmonary site, enter the sample collection date. If known, specify species and serogroup.
Antibody titer: If there was a fourfold or greater rise in specific serum antibody titer to Legionella pneumophila serogroup 1, enter the sample collection dates for the initial (acute) and convalescent titer. Both acute and convalescent titers are necessary to fulfill this criterion. Must have paired sera collected at acute onset to 2 weeks after symptoms and 3 to 6 weeks later.*
Nucleic acid assay (e.g., polymerase chain reaction or PCR): If the laboratory detects Legionella species by a validated nucleic acid assay, such as PCR, enter the sample collection date and indicate sample site. If known, specify species and serogroup.
Suspect Case
Antibody titer: If there was a fourfold or greater rise in antibody titer to specific species or serogroups of Legionella other than Legionella pneumophila serogroup 1 or to multiple species or serogroups of Legionella using pooled antigen, enter the sample collection dates for the initial (acute) and convalescent titer. If known, specify species and serogroup. Both acute and convalescent titers are necessary to fulfill this criterion. Must have paired sera collected at acute onset to 2 weeks after symptoms and 3 to 6 weeks later.*
Direct fluorescent antibody (DFA) or immunohistochemistry (IHC): If the laboratory detects specific Legionella antigen or staining of the organism in respiratory secretions, lung tissue, or pleural fluid by DFA or IHC, enter the sample collection date and indicate sample site. If known, specify species and serogroup.
Probable Case
Check this box if the case has clinically compatible symptoms, an epidemiologic link in the 14 days before disease onset, but no Legionella laboratory testing. Indicate the nature of the epidemiologic link the Comments field.
Comments: Use this space to provide additional information or expand on areas in the form where there was not enough room.
*The CSTE case definition does not specify timing for acute and convalescent sera collection. The timing of sera collection is in accordance with McDade et. al. 1977.1
Reference
- McDade JE, Shepard CC, Fraser DW, Tsai TR, Redus MA, Dowdle WR. Legionnaires' disease: isolation of a bacterium and demonstration of its role in other respiratory disease. N Engl J Med. 1977;297(22):1197–1203.
