At a glance
During March 28-May 14, 2023, CDC conducted an opt-in Internet panel survey of 3,437 U.S. HCP to estimate influenza coverage during the 2022-2023 influenza season as well as receipt of the primary COVID-19 vaccination series and a COVID-19 bivalent vaccine. Overall, 75.9% of HCP reported receiving influenza vaccination during the 2022-2023 season.
Summary
The Advisory Committee on Immunization Practices (ACIP) recommends that all health care personnel (HCP) receive an annual influenza vaccination to reduce influenza-related morbidity and mortality among HCP and their patients.1 ACIP also recommends that all persons aged ≥6 months, including HCP, be vaccinated with COVID-19 vaccines and remain up to date.23 During March 28-May 14, 2023 CDC conducted an opt-in Internet panel survey of 3,437 U.S. HCP to estimate influenza coverage during the 2022-2023 influenza season as well as receipt of the primary COVID-19 vaccination series and a COVID-19 bivalent vaccine. Overall, 75.9% of HCP reported receiving influenza vaccination during the 2022-2023 season, 84.1% reported having completed the primary COVID-19 vaccination series, and 38.6% reported receiving a COVID-19 bivalent vaccine. Among HCP, influenza, COVID-19 primary series, and COVID-19 bivalent vaccination coverage were lowest among assistants and aides and those whose employer neither required nor recommended the vaccines. Influenza and COVID-19 primary series vaccination coverage were lowest among those working in long-term care facilities (LTC) and home health care settings, and COVID-19 bivalent vaccination coverage was lowest among those working in other clinical settings. Influenza vaccination coverage during the 2022-2023 season was highest among physicians (94.5%) and HCP who worked in hospital settings (85.7%), similar to previous seasons. Maximizing HCP influenza and COVID-19 vaccination uptake among HCP and patients in the upcoming season is important to reduce influenza and COVID-19 related morbidity and mortality among HCP and their patients and decrease absenteeism among HCP due to respiratory illness. Workplace requirements for influenza and COVID-19 vaccination and providing vaccines onsite could increase vaccination coverage.
Methods
An Internet panel survey of HCP was conducted from March 28, 2023-May 14, 2023, to provide estimates of influenza and COVID-19 vaccination coverage among HCP during the 2022-23 influenza season. Similar annual surveys have been conducted since the 2010-11 influenza season.45 Respondents were recruited from two preexisting national opt-in Internet sources: MedscapeA*, a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by Dynata†B. Responses were weighted to the distribution of the U.S. population of HCP§C by occupation¶D, age, sex, race and ethnicity, work setting, and U.S. Census Bureau region. A poststratification weight for each responding person in the survey was calculated by fitting a generalized exponential model and estimating the model parameters using calibration equations.6 Among 3,709 eligible participants, a total of 3,528 completed the survey (completion rate=95.1%**E). Eighty-nine participants were excluded because they indicated working in a setting other than those listed, and the verbatim description did not qualify as a health care setting, and two participants were excluded because they did not provide a reliable response for the influenza vaccination question, leaving 3,437 respondents in the analytic sample.
Weighted proportions and corresponding 95% confidence intervals (CIs) for three vaccination measures (influenza vaccination coverage for the 2022-23 season and COVID-19 vaccination coverage [i.e., completion of primary series††F and receipt of bivalent vaccination§§G]) were estimated for each work setting, occupation, and demographic characteristic. Long-term care (LTC) and home health care settings include nursing homes, assisted living facilities, other long-term care facilities, home health agencies, and home health care. Employer requirements for all three vaccination measures were assessed through three separate questions¶¶H. Annual influenza vaccination coverage was additionally estimated for all work settings and occupations for the past nine seasons to compare results from 2013-2014 influenza season through 2022-2023 season to examine trends in HCP influenza coverage over time, by occupation and work setting. The Korn-Graubard method was used to calculate CIs for proportions, assuming that the weighted estimates were approximately unbiased***I. CDC's National Center for Health Statistics reliability criteria for proportions were applied to the estimates in the descriptive analyses of HCP characteristics and main reasons for not getting a COVID-19 bivalent vaccination.7 T-tests were used to assess differences in the estimated influenza and COVID-19 vaccination coverage between subgroups. Rao-Scott chi-square testing was used to assess differences in the estimated influenza vaccination coverage between seasons; p<0.05 was considered statistically significant. SAS/STAT survey procedures (version 9.4; SAS Institute) were used to conduct all analyses.
Estimated (weighted) proportions and corresponding confidence intervals (CIs) for vaccination coverage are presented by each work setting, occupation, demographic characteristics, and influenza vaccination status for the 2020-21 season. The Korn-Graubard method was used to calculate confidence intervals for proportions, assuming that the weighted estimates are approximately unbiased.¶D The National Center for Health Statistics (NCHS) reliability criteria for proportions were applied to the estimates in the descriptive analyses of HCP characteristics, reasons for getting and not getting an influenza vaccine, and for the attitudes toward influenza vaccine and illness.8 Chi-square testing was utilized to assess differences in the estimated influenza vaccination coverage between subgroups and the responses to attitudes questions. SAS 9.4 (Cary, NC) and SAS-callable SUDAAN software (version 11.0.1; RTI International) were used to conduct all analyses.
Results
Overall, 75.9% of HCP reported having received an influenza vaccination during the 2022-2023 season, lower than the 80.6% reported in the 2021-2022 season (p<0.05) (Table 1). Among all HCP, influenza vaccination coverage over the previous nine seasons steadily increased from the 2013-2014 season through the 2018-2019 seasons, and then decreased between the 2019-2020 and 2020-2021 seasons and between the 2021-2022 and 2022-2023 seasons after an apparent increase in 2021-2022. Similar patterns were seen for HCP working in ambulatory care and other clinical settings, while coverage among HCP working in hospitals declined from a high of 95.2% in 2018-2019 to 85.7% in 2022-23, and coverage among HCP working in LTC settings has remained stable from 2015-2016 through 2022-2023 (Figure 1). As in previous seasons, influenza vaccination coverage in 2022-2023 was highest among HCP working in hospitals (85.7%) and lowest among HCP working in LTC and home health care settings (68.3%) (Table 1, Figure 1). Influenza vaccination coverage was highest among physicians (94.5%), pharmacists (90.7%), nurse practitioners and physician assistants (91.0%) and nurses (88.1%), and lower among other clinical personnel (82.5%), non-clinical personnel (70.6%), and assistants/aides (62.8%); similar patterns were seen in previous seasons (Table 1, Figure 2). Estimates and 95% CIs for influenza seasons 2013-2014 through 2022-2023 are reported in the Supplementary Table S1.
Table 1. Receipt of influenza vaccination among health care personnel by selected characteristics — Internet Panel Surveys*, United States, April 2022 and April 2023
| 2021–22 Influenza season† | 2022–23 Influenza season |
|
|||
| Characteristic | Number (weighted %) | Weighted % vaccinated
(95% CI) |
Number (weighted %) | Weighted % vaccinated
(95% CI) |
Percentage point change in weighted % vaccinated, 2021-2022 to 2022-2023 (95% CI) |
| Total/Overall | 3,618 | 80.6 (77.4, 83.5) | 3,437 | 75.9 (73.1, 78.6) | -4.7 (-8.7, -0.6)¶ |
| Age group, years | |||||
| 18-29 years (ref) | 343 (16.2) | 73.5 (61.5, 83.5) | 422 (15.8) | 72.7 (65.5, 79.2) | -0.8 (-13.2, 11.6) |
| 30-45 years | 1,616 (42.0) | 83.5 (78.5, 87.7) | 1,585 (43.2) | 72.6 (67.4, 77.4) | -10.9 (-17.5, -4.3)¶ |
| 45-60 years | 1,112 (28.2) | 78.5 (74.0, 82.4) | 979 (28.1) | 78.5 (73.9, 82.6) | 0.0 (-5.8, 5.9) |
| 60+ years | 547 (13.6) | 84.5 (77.2, 90.1) | 449 (12.9) | 85.3 (79.3, 90.1) ** | 0.8 (-7.2, 8.8) |
| Race/ethnicity†† | |||||
| White, non-Hispanic (ref) | 2,329 (64.6) | 81.5 (77.1, 85.3) | 2,164 (60.1) | 76.2 (72.3, 79.9) | -5.2 (-10.6, 0.2) |
| Black, non-Hispanic | 319 (13.4) | 76.9 (69.3, 83.4) | 405 (15.3) | 70.4 (62.6, 77.3) | -6.5 (-16.4, 3.3) |
| Hispanic | 485 (12.8) | 79.9 (70.4, 87.5) | 503 (15.1) | 78.8 (72.2, 84.4) | -1.1 (-11.2, 8.9) |
| Other, non-Hispanic | 471 (9.2) | 80.7 (72.7, 87.2) | 361 (9.4) | 79.0 (69.0, 87.0) | -1.6 (-12.6, 9.3) |
| Gender | |||||
| Male (Ref) | 1,081 (30.9) | 89.2 (84.7, 92.7) | 789 (30.6) | 78.7 (70.6, 85.4) | -10.5 (-18.5, -2.4)¶ |
| Female | 2,537 (69.1) | 76.7 (72.9, 80.3) ** | 2,619 (68.6) | 70.4 (62.6, 77.3) | -2.0 (-6.4, 2.3) |
| Transgender, non-binary, or another gender | 29 (0.8) | __§§ | |||
| Education | |||||
| Some college education or less (ref) | 526 (26.0) | 66.6 (59.0, 73.5) | 1,035 (27.1) | 63.4 (56.7, 69.7) | -3.2 (-12.6, 6.3) |
| Associate or bachelor’s degree | 1,038 (47.0) | 82.0 (77.0, 86.3) ** | 1,113 (47.2) | 79.4 (75.4, 83.0) ** | -2.7 (-8.5, 3.2) |
| Master’s, professional, or doctoral degree | 2,053 (27.0) | 91.5 (88.9, 93.8) ** | 1,289 (25.8) | 82.8 (78.2, 86.7) ** | -8.8 (-13.5, -4.0)¶ |
| Occupation¶¶ | |||||
| Physician (ref) | 591 (3.3) | 96.6 (94.4, 98.2) | 354 (3.5) | 94.5 (90.1, 97.3) | -2.2 (-5.9, 1.6) |
| Nurse practitioner / Physician assistant | 333 (1.6) | 92.2 (88.6, 95.0)** | 219 (1.6) | 91.0 (86.2, 94.5) | -1.2 (-6.2, 3.7) |
| Nurse | 362 (18.5) | 86.8 (81.6, 90.9)** | 217 (18.2) | 88.1 (81.7, 92.9)** | 1.3 (-5.6, 8.2) |
| Pharmacist | 509 (1.4) | 94.4 (92.0, 96.2) | 322 (1.3) | 90.7 (86.8, 93.7) | -3.8 (-7.6, 0.0) |
| Other clinical personnel*** | 916 (20.9) | 86.8 (83.0, 89.9)** | 601 (21.0) | 82.5 (77.3, 86.9)** | -4.3 (-10.0, 1.4) |
| Assistant/aide | 540 (24.2) | 69.1 (64.6, 73.3) ** | 1,083 (23.7) | 62.8 (59.3, 66.1) ** | -6.3 (-11.7, -0.9)¶ |
| Non-clinical personnel|| | 333 (30.1) | 78.6 (68.8, 86.6) ** | 612 (30.5) | 70.6 (62.8, 77.6) ** | -8.1 (-19.1, 3.0) |
| Work setting§§§ | |||||
| Hospital | 1,488 (40.1) | 92.2 (89.4, 94.4)** | 1,125 (39.4) | 85.7 (81.3, 89.4)** | -6.5 (-11.1, -1.9)¶ |
| Ambulatory care | 1,335 (31.7) | 81.4 (76.9, 85.3) | 1,083 (32.4) | 75.3 (70.9, 79.4) | -6.0 (-11.8, -0.2)¶ |
| Long-term care facility / home health care¶¶¶ |
648 (28.6) | 67.9 (59.6, 75.4)** | 1,029 (28.1) | 68.3 (61.4, 74.5)** | 0.3 (-9.6, 10.3) |
| Other clinical setting‡‡ | 783 (10.2) | 80.4 (73.0, 86.4) | 674 (11.9) | 68.5 (61.3, 75.0)** | -11.9 (-21.1, -2.7)¶ |
| Location of primary workplace†††† | |||||
| Rural | 496 (13.9) | 76.7 (71.0, 81.7) | 555 (15.2) | 65.1 (53.9, 75.3) | -11.6 (-23.1, -0.0)¶ |
| Non-rural | 3,117 (86.1) | 81.3 (77.6, 84.5) | 2,876 (84.8) | 77.7 (75.1, 80.2)** | -3.5 (-7.7, 0.7) |
| U.S. Census Bureau region§§§§ | |||||
| Northeast (ref) | 791 (17.5) | 86.7 (82.1, 90.4) | 661 (17.8) | 79.3 (73.0, 84.7) | -7.4 (-14.2, -0.5)¶ |
| Midwest | 816 (22.9) | 83.2 (78.7, 87.2) | 781 (22.0) | 75.0 (69.4, 80.1) | -8.2 (-14.8, -1.6)¶ |
| South | 1,251 (37.0) | 76.5 (69.7, 82.4)** | 1,299 (37.6) | 75.5 (69.9, 80.5) | -1.0 (-8.9, 7.0) |
| West | 760 (22.5) | 79.9 (73.0, 85.7) | 690 (22.6) | 74.4 (68.1, 80.0) | -5.5 (-13.9, 2.9) |
| Employer influenza vaccination requirement | |||||
| Required (ref) | 1,714 (44.2) | 95.2 (89.8, 98.3) | 1,345 (41.6) | 95.9 (93.6, 97.5) | 0.6 (-3.6, 4.9) |
| Recommended | 1,293 (35.0) | 77.1 (71.4, 82.2)** | 1,316 (38.8) | 70.2 (64.2, 75.8)** | -6.9 (-14.6, 0.8) |
| Not required or recommended | 611 (20.8) | 55.2 (44.0, 66.1)** | 776 (19.6) | 44.8 (38.9, 50.9)** | -10.4 (-22.6, 1.7) |
| Receipt of ≥1 dose of a COVID-19 vaccine | |||||
| Yes | 3,361 (89.6) | 86.5 (83.5, 89.1)** | 2,959 (87.0) | 83.8 (81.4, 86.0)** | -2.7 (-6.2, 0.8) |
| No | 257 (10.4) | 29.6 (18.4, 43.0) | 476 (13.0) | 23.4 (16.7, 31.2) | -6.2 (-19.9, 7.4) |
Abbreviation: Ref = referent group.
*Respondents were recruited from two preexisting national opt-in Internet sources: Medscape, a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by Dynata.
†Estimates for the 2021-22 season in this report used updated weights, which are slightly different than the report published in October 2022.
§Modified Clopper-Pearson 95% CI according to the approach of Korn and Graubard.
¶Statistically significant (p<0.05) when compared across seasons.
**Statistically significant (p<0.05) when compared with Ref in the same season.
††Race and ethnicity were self-reported. Respondents who identified as Hispanic might be of any race. The “Other” race category included persons who identified as Asian, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, and persons who selected “Other” or “multiple races.”
§Estimate does not meet CDC’s National Center for Health Statistics standards of reliability (https://www.cdc.gov/nchs/data/series/sr_02/sr02_175.pdf).
¶¶Excludes students.
***Includes dentists, allied health professionals, technicians and technologists, emergency technicians, emergency medical technicians, and paramedics.
†††Includes administrative support staff members and managers, and non-clinical support staff members.
§§Respondents could select more than one work setting. Each work setting is represented by a separate variable with two values (yes and no, where reference value is no).
¶¶¶ Nursing home, assisted living facility, other long-term care facility, home health agency, or home health care.
****Includes dentist office or dental clinic, pharmacy, emergency medical services, and other settings where clinical care or related services were provided to patients.
††††Rurality was defined using zip codes in which >50% of the population resides in a nonmetropolitan county, a rural U.S. Census Bureau tract, or both, according to the Health Resources and Services Administration’s definition of rural population. https://www.hrsa.gov/rural-health/about-us/what-is-rural
§§§https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf
Figure 1. Percentage of health care personnel who received influenza vaccination, by work setting* — Internet panel surveys†, United States, 2013-2014 through 2022-2023 influenza seasons§
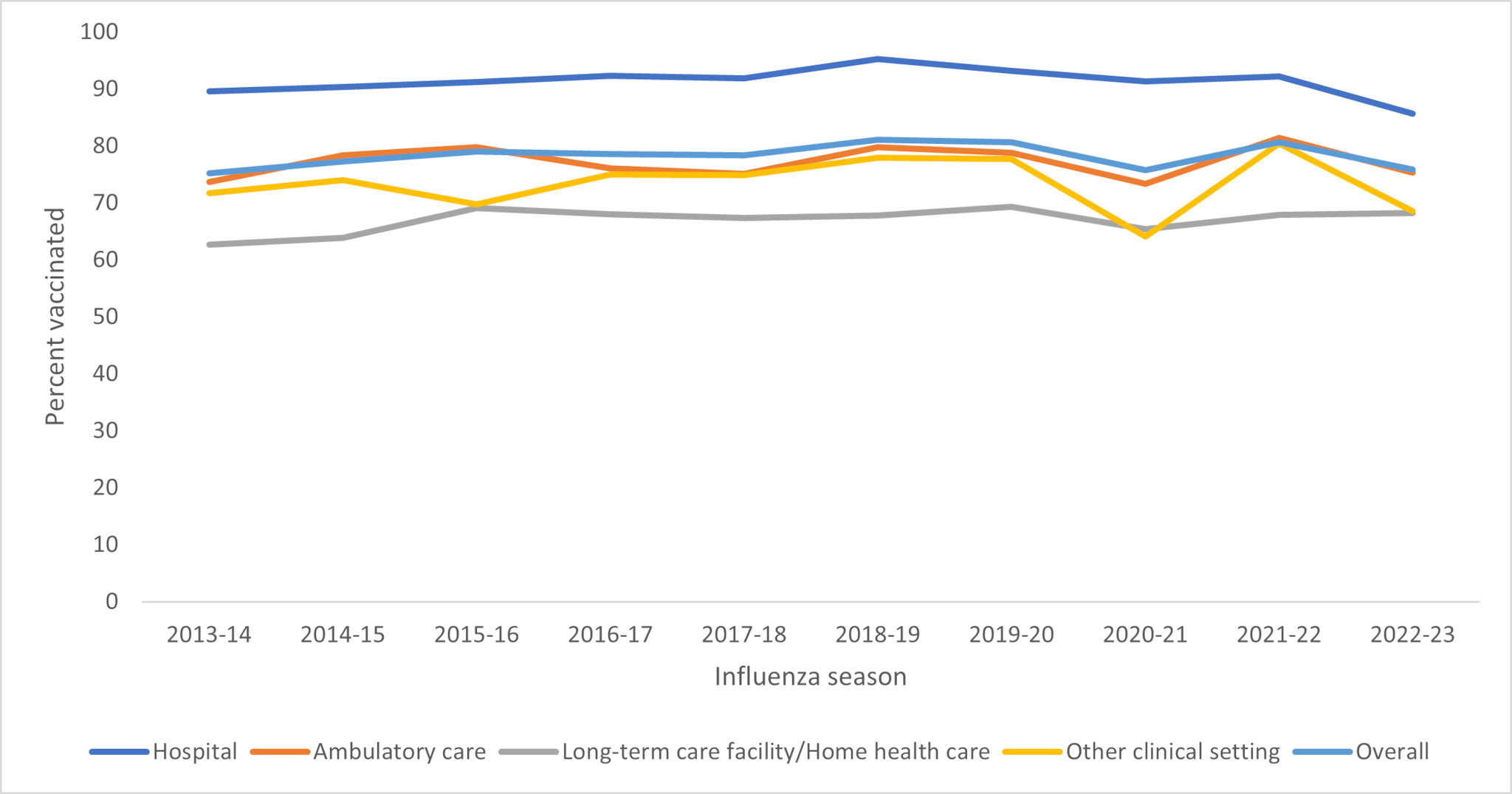
*Respondents could select more than one work setting. The other clinical setting category includes dentist office or dental clinic, pharmacy, emergency medical services, and other settings where clinical care or related services were provided to patients.
†Respondents were recruited from two preexisting national opt-in Internet sources: Medscape, a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by Dynata.
§During the 2020-2021 influenza season, a weighting methodological change was implemented. Prior to the 2020-2021 influenza season, weights were calculated to population control totals controlling for the main effects (occupation, age group, race and ethnicity, gender, work setting, and Census region); From the 2020-2021 influenza season and onward, interaction terms between occupation and the other main effects were added in the weighting model. Influenza Vaccination Coverage Among Health Care Personnel — United States, 2020–21 Influenza Season
Supplementary Table S1. Influenza vaccination coverage among health care personnel, by select characteristics — Internet panel surveys*, United States, 2013-2014 through 2022-2023 influenza seasons
| Weighted % vaccinated (95% CI)§ | ||||||||||
| Characteristic | 2013-14 | 2014-15 | 2015-16 | 2016-17 | 2017-18 | 2018-19 | 2019-20 | 2020-21 | 2021-22 | 2022-23 |
| Total | 75.2 (71.9, 78.2) | 77.3 (74.6, 79.8) | 79.0 (76.6, 81.3) | 78.6 (76.0, 81.0) | 78.4 (76.0, 80.8) | 81.1 (78.6, 83.4) | 80.6 (78.2, 82.8) | 75.7 (70.7, 80.3) | 80.6 (77.4, 83.5) | 75.9 (73.1, 78.6) |
| Occupation¶ | ||||||||||
| Physician | 92.2 (88.7, 94.9) | 88.9 (84.5, 92.4) | 95.6 (92.0, 97.9) | 95.8 (92.5, 97.9) | 96.1 (92.2, 98.4) | 96.7 (93.5, 98.6) | 98.0 (95.3, 99.4) | 90.8 (83.7, 95.6) | 96.6 (94.4, 98.2) | 94.5 (90.1, 97.3) |
| Nurse practitioner/Physician assistant | 89.6 (82.9, 94.3) | 87.0 (80.9, 91.8) | 90.3 (84.0, 94.7) | 92.0 (86.0, 96.0) | 87.8 (79.7, 93.5) | 91.0 (82.0, 96.4) | 88.8 (80.9, 94.2) | 91.9 (83.5, 96.8) | 92.2 (88.6, 95.0) | 91.0 (86.2, 94.5) |
| Nurse | 90.5 (84.9, 94.5) | 89.0 (83.1, 93.4) | 90.1 (84.4, 94.3) | 92.6 (87.3, 96.2) | 90.5 (85.1, 94.5) | 91.8 (86.1, 95.7) | 92.0 (86.9, 95.5) | 90.8 (82.5, 96.0) | 86.8 (81.6, 90.9) | 88.1 (81.7, 92.9) |
| Pharmacist | 85.7 (74.3, 93.4) | 95.3 (88.1, 98.8) | 86.5 (74.8, 94.1) | 93.7 (90.2, 96.2) | 92.2 (87.9, 95.4) | 91.5 (86.9, 94.8) | 90.6 (86.4, 93.8) | 90.7 (86.9, 93.7) | 94.4 (92.0, 96.2) | 90.7 (86.8, 93.7) |
| Other clinical personnel** | 87.4 (83.4, 90.7) | 81.3 (76.7, 85.4) | 84.7 (80.7, 88.2) | 80.0 (75.6, 84.0) | 80.9 (75.3, 85.6) | 85.8 (81.0, 89.8) | 81.7 (76.6, 86.1) | 84.0 (77.4, 89.4) | 86.8 (83.0, 89.9) | 82.5 (77.3, 86.9) |
| Assistant/Aide | 57.7 (49.0, 66.0) | 64.4 (58.5, 69.9) | 64.1 (60.1, 67.9) | 69.1 (65.2, 72.9) | 71.1 (66.7, 75.2) | 72.5 (68.2, 76.5) | 72.4 (68.3, 76.1) | 64.0 (59.5, 68.4) | 69.1 (64.6, 73.3) | 62.8 (59.3, 66.1) |
| Non-clinical personnel†† | 68.6 (62.2, 74.6) | 75.2 (69.2, 80.5) | 77.7 (71.9, 82.8) | 73.7 (67.3, 79.5) | 72.8 (67.1, 77.9) | 75.5 (69.5, 80.8) | 76.7 (71.0, 81.8) | 67.0 (52.8, 79.3) | 78.6 (68.8, 86.6) | 70.6 (62.8, 77.6) |
| Work setting§§ | ||||||||||
| Hospital | 89.6 (86.2, 92.4) | 90.4 (86.6, 93.3) | 91.2 (88.1, 93.8) | 92.3 (89.0, 94.8) | 91.9 (88.4, 94.6) | 95.2 (92.7, 97.0) | 93.2 (89.9, 95.6) | 91.3 (87.7, 94.2) | 92.2 (89.4, 94.4) | 85.7 (81.3, 89.4) |
| Ambulatory care | 73.7 (67.1, 79.6) | 78.4 (74.2, 82.2) | 79.8 (74.9, 84.2) | 76.1 (71.2, 80.5) | 75.1 (69.8, 79.9) | 79.8 (74.8, 84.1) | 78.8 (74.1, 82.9) | 73.3 (59.1, 84.6) | 81.4 (76.9, 85.3) | 75.3 (70.9, 79.4) |
| Long-term care facility/Home health care¶¶ | 63.0 (56.1, 69.6) | 63.9 (58.0, 69.6) | 69.2 (64.6, 73.6) | 68.0 (62.2, 73.4) | 67.4 (62.5, 71.9) | 67.9 (62.5, 73.0) | 69.3 (64.1, 74.2) | 65.4 (58.9, 71.6) | 67.9 (59.6, 75.4) | 68.3 (61.4, 74.5) |
| Other clinical setting*** | 71.7 (61.9, 80.1) | 74.0 (65.2, 81.5) | 69.8 (61.3, 77.4) | 75.0 (68.3, 80.9) | 74.9 (67.8, 81.1) | 77.9 (70.2, 84.5) | 77.7 (71.1, 83.5) | 64.1 (54.0, 73.3) | 80.4 (73.0, 86.4) | 68.5 (61.3, 75.0) |
Abbreviations: Ref = referent group.
*Completion of primary series of COVID-19 vaccines was defined as the receipt of a 2-dose primary mRNA COVID-19 vaccine series for respondents who did not report being immunocompromised, or an additional dose after completion of a 2-dose mRNA COVID-19 vaccine series for respondents who reported being immunocompromised. For respondents whose initial vaccine was Janssen (Johnson & Johnson), completion of primary COVID-19 series was defined as the receipt of 1 dose for those who were not immunocompromised, or a second COVID-19 vaccine (either Janssen or mRNA) for those who were immunocompromised.
†Respondents were considered to have received a COVID-19 bivalent booster vaccine if they responded "Yes" to the question, "Have you received a bivalent booster vaccine?" which was asked of respondents who reported receipt of at least one dose of a COVID-19 vaccine.
§Respondents were recruited from two preexisting national opt-in Internet sources: Medscape, a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by Dynata.
¶Modified Clopper-Pearson 95% CI according to the approach of Korn and Graubard.
**Statistically significant (p<0.05) when compared with Ref.
††Race and ethnicity were self-reported. Respondents who identified as Hispanic might be of any race. The “Other” race category included persons who identified as Asian, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, and persons who selected “Other” or “multiple races.”
§Estimate does not meet CDC’s National Center for Health Statistics standards of reliability (https://www.cdc.gov/nchs/data/series/sr_02/sr02_175.pdf).
¶¶Excludes students (29).
*** Includes dentists, allied health professionals, technicians and technologists, emergency technicians, emergency medical technicians, and paramedics.
†††Includes administrative support staff members and managers, and nonclinical support staff members.
§§Respondents could select more than one work setting. Each work setting is represented by a separate variable with two values (yes and no, where reference value is no).
¶¶¶Nursing home, assisted living facility, other long-term care facility, home health agency, or home health care.
****Includes dentist office or dental clinic, pharmacy, emergency medical services, and other settings where clinical care or related services were provided to patients.
††††Rurality was defined using zip codes in which >50% of the population resides in a nonmetropolitan county, a rural U.S. Census Bureau tract, or both, according to the Health Resources and Services Administration’s definition of rural population. https://www.hrsa.gov/rural-health/about-us/what-is-rural.
§§§https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf
Figure 2. Percentage of health care personnel who received influenza vaccination, by occupation* — Internet panel surveys†, United States, 2013-2014 through 2022-2023 influenza seasons§
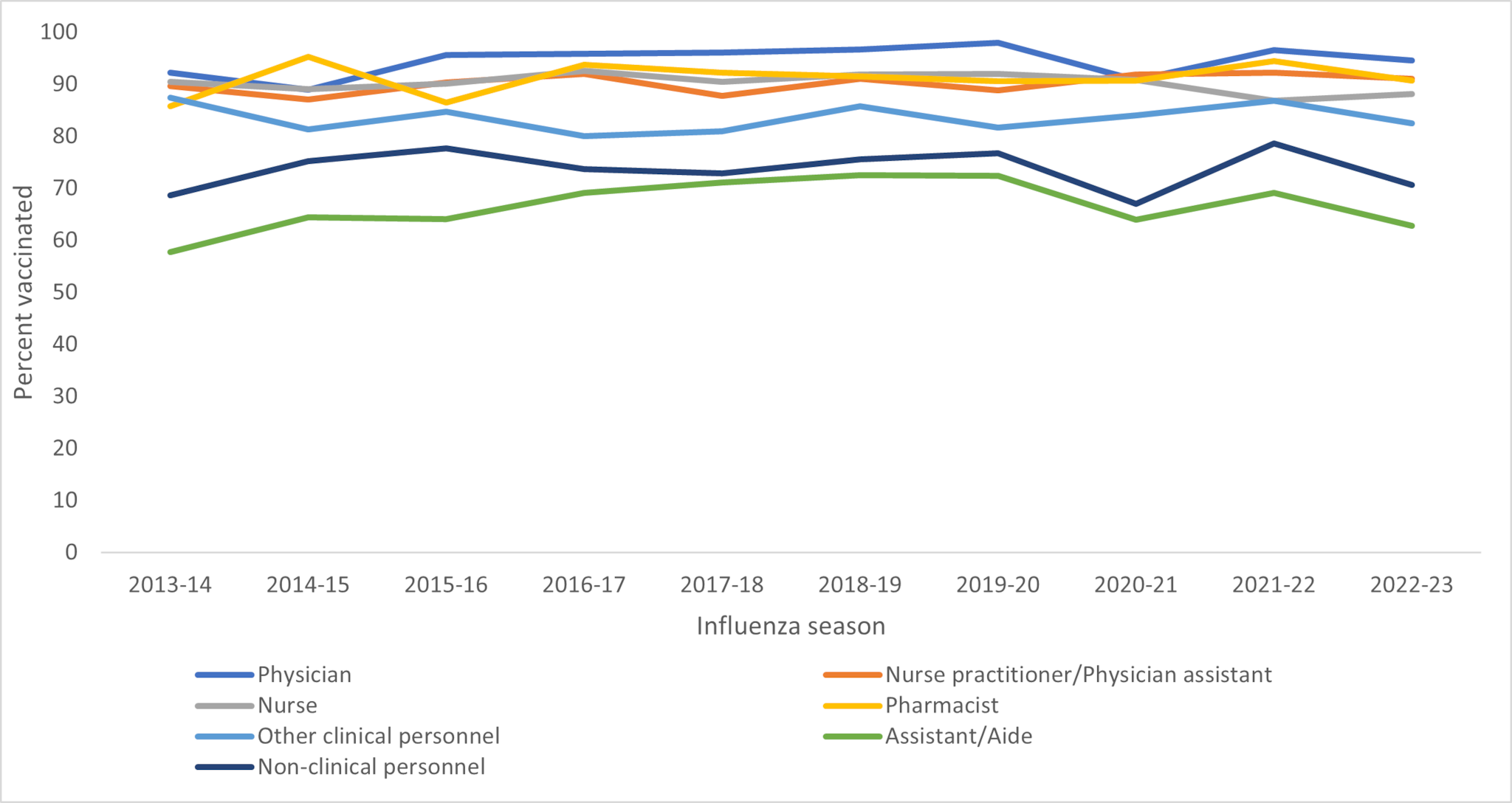
*Other clinical personnel includes dentists, allied health professionals, technicians and technologists, emergency medical technicians, and paramedics. Non-clinical personnel includes administrative support staff members and managers, and non-clinical support staff members.
†Respondents were recruited from two preexisting national opt-in Internet sources: Medscape, a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by Dynata.
†During the 2020-2021 influenza season, a major weighting methodological change was implemented. Prior to the 2020-2021 influenza season, weights were calculated to population control totals controlling for the main effects (occupation, age group, race and ethnicity, gender, work setting, and Census region); From the 2020-2021 influenza season and onward, interaction terms between occupation and the other main effects were added in the weighting model. Influenza Vaccination Coverage Among Health Care Personnel — United States, 2020–21 Influenza Season.
During the 2022-2023 season, higher influenza vaccination coverage was reported among HCP with either a master's, professional, or doctoral degree (82.8%) than among those with some college education or less (63.4%). Coverage was highest among HCP who reported an employer requirement for influenza vaccination (95.9%) than among those who reported an employer recommendation (70.2%) or no recommendation or requirement for vaccination (44.8%). Influenza vaccination coverage was also highest among HCP who were aged ≥60 years (85.3%), reported working in a non-rural area (77.7%), and HCP who reported receiving ≥1 dose of COVID-19 vaccine (83.8%). Compared with the 2021-2022 influenza season, statistically significant decreases in influenza vaccination coverage were observed among HCP aged 30-44 years (10.9 percentage points), male (10.5 percentage points), those with master's, professional, or doctoral degrees (8.8 percentage points), assistants/aides (6.3 percentage points), those who work in hospital (6.5 percentage points), ambulatory (6.0 percentage points), and other clinical settings (11.9 percentage points), those working in rural areas (11.6 percentage points), and those who worked in the Midwest (8.2 percentage points) and Northeast (7.4 percentage points) regions (Table 1).
Overall, 84.1% of HCP reported having completed the COVID-19 primary series vaccination and 38.6% reported having received a COVID-19 bivalent vaccine (Table 2). Completion of COVID-19 primary series vaccination was highest among those aged ≥60 years (91.0%), pharmacists (96.0%) and physicians (95.4%), HCP working in a hospital setting (91.2%), and those who reported ever having COVID-19 (85.0%). COVID-19 primary series vaccination coverage was also higher among HCP who reported an employer requirement for COVID-19 vaccination (92.2%) than among those who reported an employer recommendation (81.0%), or no recommendation or requirement (58.8%). Receipt of a COVID-19 bivalent vaccination among all HCP was highest among HCP aged ≥60 years (60.1%), physicians (54.9%), HCP working in hospital settings (41.1%), and those who reported an employer requirement for COVID-19 bivalent vaccine (67.7%). COVID-19 bivalent vaccination coverage was lowest among HCP aged 30-44 years (32.4%), non-Hispanic Black (29.4%), those with some college education or less (28.3%), assistants/aides (27.3%), HCP working in other clinical settings (34.2%), and HCP who reported ever having COVID-19 (35.7%) (Table 2).
Table 2. Completion of primary series* of a COVID-19 vaccine and receipt of a bivalent vaccine† among health care personnel, by selected characteristics — Internet panel surveys§, United States, April 2023
| Weighted % (95% CI)¶ | |||
| Characteristic | Total no. (weighted %) (N = 3,437) | Completion of primary COVID-19 vaccination series (N = 3,437) | Receipt of bivalent vaccine (N = 3,437) |
| Total | 3,437 | 84.1 (81.5, 86.5) | 38.6 (35.4, 41.8) |
| Age group, years | |||
| 18-29 (Ref) | 420 (15.7) | 78.7 (72.4, 84.1) | 33.9 (25.5, 43.2) |
| 30-44 | 1,585 (43.2) | 81.4 (76.2, 86.0) | 32.4 (27.8, 37.3) |
| 45-59 | 981 (28.2) | 88.0 (84.5, 91.0)** | 40.7 (34.9, 46.7) |
| 60+ | 449 (12.9) | 91.0 (85.8, 94.8)** | 60.1 (51.6, 68.2)** |
| Race and ethnicity†† | |||
| White, non-Hispanic (Ref) | 2,165 (60.2) | 83.1 (79.1, 86.6) | 38.2 (34.3, 42.1) |
| Black, non-Hispanic | 405 (15.3) | 80.7 (75.0, 85.6) | 29.4 (22.1, 37.6)** |
| Hispanic | 502 (15.1) | 86.8 (81.2, 91.2) | 43.1 (33.4, 53.1) |
| Other, non-Hispanic | 361 (9.4) | 92.7 (88.8, 95.5)** | 49.2 (38.4, 60.0) |
| Gender | |||
| Male (Ref) | 789 (30.6) | 88.2 (80.0, 93.9) | 43.9 (36.5, 51.4) |
| Female | 2,619 (68.6) | 82.1 (79.8, 84.3) | 36.0 (32.8, 39.4) |
| Transgender, non-binary, or another gender | 29 (0.8) | __§§ | __§§ |
| Education | |||
| Some college education or less (ref) | 1,034 (27.0) | 70.7 (64.0, 76.9) | 28.3 (22.7, 34.4) |
| Associate or bachelor’s degree | 1,114 (47.2) | 86.5 (82.9, 89.6)** | 37.7 (32.7, 42.8)** |
| Master’s, professional, or doctoral degree | 1,289 (25.8) | 93.8 (91.1, 95.8)** | 51.1 (45.6, 56.5)** |
| Occupation¶¶ | |||
| Physician (ref) | 354 (3.5) | 95.4 (91.4, 97.8) | 54.9 (48.0, 61.6) |
| Nurse practitioner/ Physician assistant | 219 (1.6) | 93.7 (89.5, 96.5) | 49.2 (41.8, 56.7) |
| Nurse | 217 (18.3) | 92.5 (86.3, 96.5) | 45.1 (36.6, 53.9) |
| Pharmacist | 322 (1.3) | 96.0 (93.2, 97.8) | 50.8 (44.3, 57.2) |
| Other clinical personnel*** | 601 (21.0) | 90.9 (86.3, 94.4) | 39.8 (32.9, 46.9)** |
| Assistant/aide | 1,083 (23.7) | 71.2 (68.1, 74.2)** | 27.3 (24.1, 30.6)** |
| Non-clinical personnel††† | 612 (30.5) | 81.9 (74.2, 88.2)** | 39.5 (32.2, 47.2)** |
| Work setting§§§ | |||
| Hospital | 1,126 (39.4) | 91.2 (87.6, 94.1)** | 41.1 (35.6, 46.7) |
| Ambulatory care | 1,083 (32.4) | 86.0 (82.5, 89.1) | 39.1 (34.0, 44.3) |
| Long-term care facility/Home health care¶¶¶ | 1,028 (28.1) | 74.9 (68.0, 80.9)** | 39.4 (33.3, 45.7) |
| Other clinical setting‡‡ | 674 (12.0) | 81.6 (75.6, 86.7) | 34.2 (26.9, 42.1) |
| Location of primary workplace†††† | |||
| Rural (Ref) | 556 (15.2) | 72.6 (60.6, 82.6) | 30.3 (21.8, 39.9) |
| Non-rural | 2,875 (84.8) | 86.4 (84.3, 88.3)** | 40.1 (36.7, 43.5)** |
| U.S. Census Bureau region§§§§ | |||
| Northeast (Ref) | 661 (17.8) | 89.3 (84.2, 93.2) | 42.9 (35.7, 50.3) |
| Midwest | 781 (22.0) | 81.8 (77.1, 85.9)** | 34.6 (28.6, 40.9) |
| South | 1,299 (37.6) | 80.8 (75.1, 85.8)** | 32.9 (27.6, 38.5)** |
| West | 690 (22.6) | 88.5 (84.0, 92.1) | 48.5 (41.7, 55.3) |
| Employer COVID-19 vaccination recommendation | |||
| Required (Ref) | 1,731 (52.6) | 92.2 (89.5, 94.4) | 41.7 (37.2, 46.3) |
| Recommended | 1,189 (34.9) | 81.0 (74.9, 86.1)** | 40.5 (34.9, 46.4) |
| Not required or recommended | 517 (12.5) | 58.8 (51.4, 66.0)** | 20.0 (14.2, 26.8)** |
| Employer bivalent vaccination recommendation | |||
| Required (Ref) | 402 (12.1) | 86.9 (79.8, 92.2) | 67.7 (58.1, 76.3) |
| Recommended | 1,582 (47.8) | 87.0 (82.0, 91.0) | 49.4 (44.4, 54.5)** |
| Not required or recommended | 1,453 (40.1) | 79.8 (76.5, 82.9)** | 16.9 (13.8, 20.4)** |
| Receipt of influenza vaccine during 2022–23 | |||
| Yes | 2,634 (75.9) | 94.0 (92.4, 95.3)** | 47.5 (43.8, 51.3)** |
| No (Ref) | 801 (24.1) | 53.1 (46.1, 60.0) | 10.4 (6.7, 15.3) |
| Employer COVID-19 vaccination recommendation | |||
| Yes | 2,154 (60.0) | 85.0 (82.4, 87.4) | 35.7 (31.9, 39.6)** |
| No (Ref) | 1,280 (40.0) | 82.7 (77.0, 87.4) | 42.5 (37.0, 48.2) |
| Employer offered any COVID-19 vaccines onsite | |||
| Offered the primary series | 1,643 (52.6) | 89.8 (87.0, 92.2)** | 43.7 (39.1, 48.5)** |
| Offered the bivalent vaccine | 1,117 (36.1) | 87.4 (80.4, 92.6) | 47.4 (40.8, 54.0)** |
| Did not offer any COVID-19 vaccines (Ref) | 1,524 (39.0) | 78.1 (75.0, 80.9) ** | 29.1 (25.4, 33.0) ** |
COVID-19 primary series (89.8%) and bivalent vaccination coverage (47.4%) was higher among HCP who reported that their employer offered COVID-19 vaccinations onsite at the workplace (Table 2). This remained true when restricted to HCP without an employer requirement for vaccination but who were offered COVID-19 vaccination onsite (vaccination coverage 85.2% and 43.4%, respectively)
The main reasons for not getting a COVID-19 bivalent vaccination among HCP who had completed a primary vaccination series were "I am concerned about possible safety risks or side effects if I got vaccinated" (12.5%), "I had a bad reaction after a previous COVID-19 vaccination" (10.2%), and "I don't think bivalent provides any more protection than initial vaccine" (8.7%) (Figure 3).
Figure 3. Main reasons* for non-receipt of a bivalent vaccine† of COVID-19 vaccine among health care personnel (n=1,627) – Internet panel surveys§, United States, April 2023
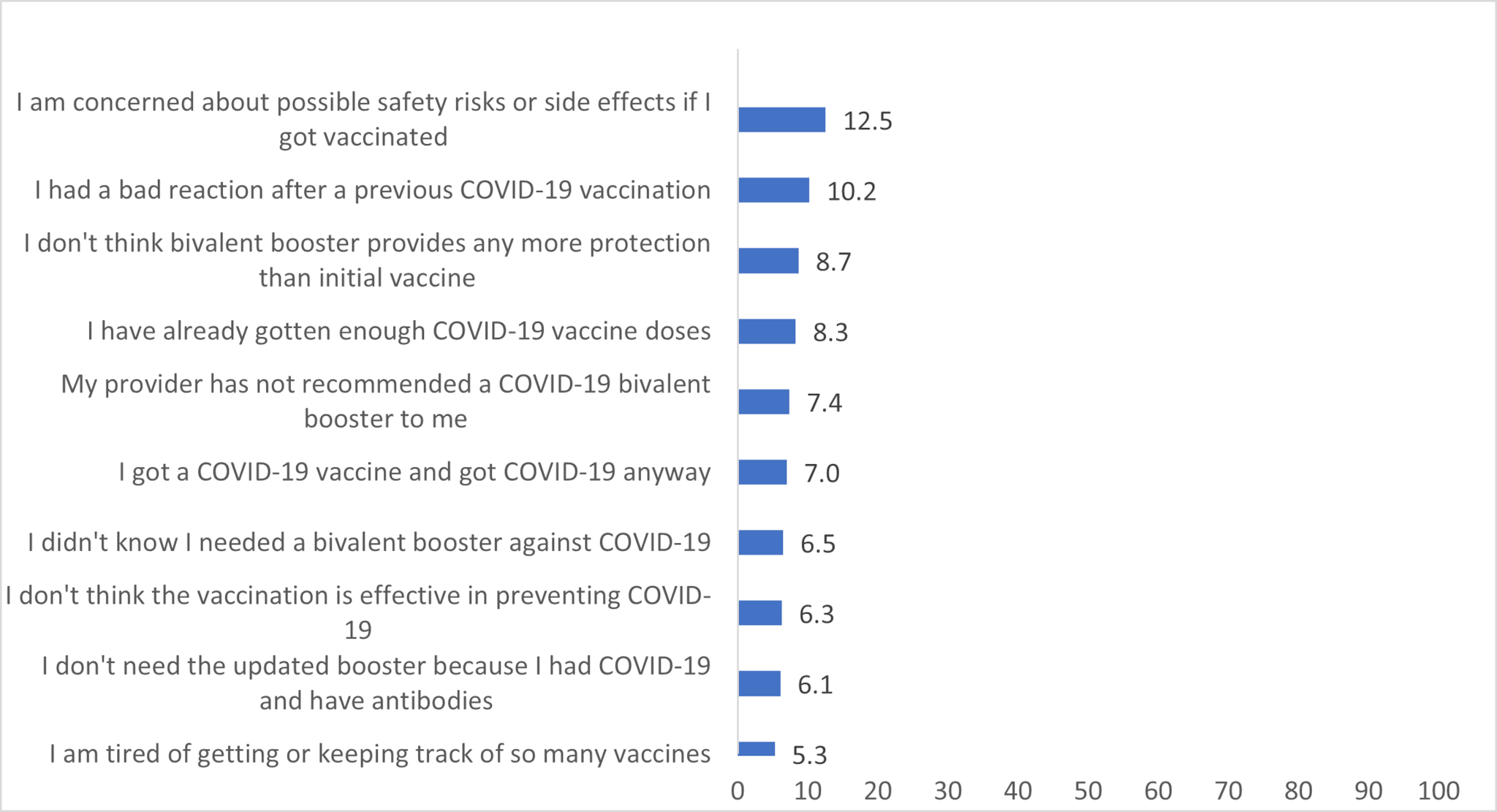
*Reasons selected by less than 5% of respondents are not presented.
†Respondents were considered to have received a COVID-19 bivalent vaccine if they responded "Yes" to the question, "Have you received a bivalent vaccine?" which was asked of respondents who reported receipt of at least one dose of a COVID-19 vaccine.
§Respondents were recruited from two preexisting national opt-in Internet sources: Medscape, a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by Dynata.
Discussion
As observed during previous influenza seasons, nonclinical personnel, assistants and aides, HCP working in LTC and home health care settings, HCP with less than a college degree, and HCP who reported their employer neither required nor recommended the influenza vaccine had the lowest vaccination coverage.45 Similar patterns were observed for COVID-19 vaccination coverage. Although coverage with the COVID-19 primary series vaccination was >70% in all work settings, more than one-half of HCP did not receive a COVID-19 bivalent vaccination and coverage was suboptimal. This may partly be because of the prioritization of HCP when the U.S. vaccination program commenced in December 2020 and a relatively high prevalence of employers required COVID-19 vaccination series among HCP.9 Comparatively, requirements for COVID-19 bivalent vaccination were infrequently reported by all HCP and coverage remained lower. Overall influenza vaccination coverage among HCP decreased in the 2020-2021 season following the COVID-19 pandemic, particularly in ambulatory and other clinical settings. Some HCP in these settings may have been working remotely or primarily conducting telehealth visits and not subject to onsite vaccination policies. After apparent recovery during the 2021-2022 season, coverage decreased again during the 2022-2023 season for unknown reasons and was similar to the 2020-2021 season.4 Continued monitoring will be necessary to understand if coverage will remain lower or will return to pre-pandemic levels.
Employer vaccination requirements were strongly associated with influenza and COVID-19 vaccination uptake among HCP. Influenza vaccination coverage was approximately 50 percentage points higher among HCP with employer vaccination requirements, compared with HCP without employer vaccination requirements or recommendations. Since vaccination coverage was lowest among HCP whose employer neither required nor recommended influenza or COVID-19 vaccination, increasing workplace vaccination policies and promotional events, such as requirements to sign a waiver or declination form if not vaccinated, or public identification of vaccinated individuals, may be effective in increasing vaccination coverage in many work settings.108 Useful resources that can help with increasing vaccination coverage among HCP include CDC's long-term care web-based toolkit which provides access to resources, strategies, and educational materials, and interventions recommended by the Community Preventive Services Task Force.108
Historically HCP working in LTC and home health care settings and assistants and aides have had lower influenza vaccination coverage. This remains consistent through the prior nine influenza seasons and during the 2022-2023 season. Prior studies have also found that HCP working in LTC settings report fewer frequent influenza vaccination requirements.48 This is especially concerning since populations in LTC and home health care settings tend to be more vulnerable and at high risk for severe influenza and COVID-19 related illnesses.11 Many LTC settings now have experience implementing COVID-19 vaccine requirements and could consider these requirements for influenza and any future COVID-19 vaccines to improve coverage.
Concerns about possible side effects or safety risks, having a bad reaction after previous COVID-19 vaccinations, and not thinking that the bivalent COVID-19 vaccination provides any more protection were the most commonly reported reasons by HCP for not getting the COVID-19 bivalent vaccine. However, all of these reasons were infrequently reported, with no particular reason reported by >12.5% of unvaccinated HCP. While not assessed in the current study, in other studies among the general adult population, many eligible respondents reported that they intended to get a bivalent vaccine, but hadn't got around to it or didn't have time.12 Providing vaccination at the worksite, coupled with employer communication about the benefits and safety of bivalent vaccination could improve bivalent COVID-19 vaccine coverage as well as future vaccines. As waning immunity from primary series and prior monovalent COVID-19 vaccine booster doses have been observed,13 it remains important that HCP stay up to date on all recommended COVID-19 vaccinations, including getting updated vaccines when indicated. Remaining up to date with all COVID-19 and influenza recommended vaccinations is important for all HCP to prevent severe disease as well as reduce morbidity and mortality among HCP and their patients.
Limitations
The findings in this report are subject to at least five limitations. First, the study used a nonprobability sample of volunteer members of Medscape and Dynata Internet panels. Responses were weighted to be representative of the U.S. population of HCP; however, some bias might remain in the coverage estimates. Second, the self-selection of respondents to the panels and to the survey might introduce selection bias if the participation in the panel or survey is related to likelihood of being vaccinated. Third, vaccination status was self-reported and might be subject to recall or social desirability bias. Fourth, insufficient sample size resulted in the coverage estimates in some subgroups not meeting the National Center for Health Statistics reliability criteria for reporting proportions. Finally, during the time of the survey (April 2023), the CDC recommended a single, bivalent mRNA dose for all vaccinated and unvaccinated individuals 5 years and older to be up to date for COVID-19 vaccinations.3 However, most of the data were captured before HCP who had not completed a primary vaccination series would have had the opportunity to receive their updated COVID-19 vaccination.
Authors
Mehreen Meghani, MPH, Zhuping Garacci, MS, Hilda Razzaghi, PhD, Marie A. de Perio, MD, A. Scott Laney, PhD, Carla L. Black, PhD
Immunization Services Division, National Center for Immunization and Respiratory Diseases, CDC; Cherokee Nation Operational Solutions; Office of the Director, National Institute for Occupational Safety and Health, CDC; Division of Respiratory Health, National Institute for Occupational Safety and Health, CDC
- *Physicians, nurse practitioners, physician assistants, nurses, dentists, pharmacists, allied health professionals, technicians, technologists, emergency medical technicians, paramedics, and students in a medical-related field were recruited from the current membership roster of Medscape. Additional information on Medscape is available at https://www.medscape.com
- †Assistants, aides, and non-clinical personnel (such as administrators, clerical support workers, janitors, food service workers, and housekeepers) were recruited from general population Internet panels operated by Dynata. Additional information on Dynata and its incentives for online survey participants is available at https://www.surveysampling.com.
- §Population control totals of U.S. HCP by occupation and work setting were obtained from the U.S. Department of Commerce Bureau of Labor Statistics' occupational employment and wage statistics (https://www.bls.gov/oes/current/oessrci.htm). Population control totals by other demographic characteristics were obtained from the Bureau of Labor Statistics' labor force statistics from the current population survey. https://www.bls.gov/cps/data.htm
- ¶Major occupational categories included physicians and dentists, nurse practitioners and physician assistants, nurses, pharmacists, other clinical personnel (including allied health professionals, technicians and technologists, and emergency medical technicians and paramedics), assistants and aides, and nonclinical personnel (including administrative support staff members and managers, and nonclinical support staff members).
- **A survey response rate requires specification of the denominator at each stage of sampling. During recruitment of an online opt-in survey sample, such as the Internet panels described in this report, these numbers are not available; therefore, a response rate cannot be calculated. Instead, the survey completion rate is provided.
- ††Completion of primary series of COVID-19 vaccines was defined as the receipt of a 2-dose primary mRNA COVID-19 vaccine series for adult respondents who did not report being immunocompromised, or an additional dose after completion of a 2-dose mRNA COVID-19 vaccine series for respondents who reported being immunocompromised. For adults respondents whose initial vaccine was Janssen (Johnson & Johnson), completion of primary COVID-19 vaccination series was defined as the receipt of 1 dose for those who were not immunocompromised, or a second COVID-19 vaccine (either Janssen or mRNA) for those who were immunocompromised (because of solid organ transplant, blood or bone marrow transplant, immune deficiencies, HIV, use of corticosteroids, or use of other immune-weakening medicines).
- §Respondents were considered to have received a COVID-19 bivalent booster vaccine if they responded "Yes" to the question, "Have you received a bivalent booster vaccine?" which was asked of respondents who reported receipt of at least one dose of a COVID-19 vaccine.
- ¶¶Questions included, "Since July 1, 2022, has your employer recommended or required that you be vaccinated for flu?," "Since December 2020, has your employer recommended or required that you be vaccinated for COVID-19?," and "Has your employer recommended or required that you be vaccinated with a COVID-19 bivalent booster vaccine?"
- ***https://www.aapor.org/AAPOR_Main/media/MainSiteFiles/NPS_TF_Report_Final_7_revised_FNL_6_22_13.pdf; https://www.aapor.org/getattachment/Education-Resources/For-Researchers/AAPOR_Guidance_Nonprob_Precision_042216.pdf
- Advisory Committee on Immunization Practices; CDC. Immunization of health-care personnel: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2011;60(No. RR-7):1–45. PMID:22108587
- CDC. Vaccines & immunizations: interim clinical considerations for use of COVID-19 vaccines currently approved or authorized in the United States. Atlanta, GA: US Department of Health and Human Services, CDC; 2022. Accessed June 29, 2023. https://www.cdc.gov/vaccines/covid-19/clinical-considerations/interim-considerations-us.html
- CDC. COVID-19: stay up to date with COVID-19 vaccines including boosters. Atlanta, GA: US Department of Health and Human Services, CDC; 2022. Accessed July 19, 2023. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html
- Razzaghi, H, Srivastav A, de Perio MA, Laney AS, Black CL. Influenza and COVID-19 Vaccination Coverage Among Health Care Personnel — United States, 2021-22. MMWR Morb Mortal Wkly Rep 2022; 71:1319-1326. DOI: http://dx.doi.org/10.15585/mmwr.mm7142a2
- Masalovich S, Razzaghi H, Duque J, et al. Influenza (flu): influenza vaccination coverage among health care personnel—United States, 2020–21 influenza season. Atlanta, GA: US Department of Health and Human Services, CDC; 2021. https://www.cdc.gov/flu/fluvaxview/hcp-coverage_1920-21-estimates.htm
- Folsom, Jr. RE, Singh AC. The generalized exponential model for sampling weight calibration for extreme values, nonresponse, and poststratification. Alexandria, VA: American Statistical Association; 2000. http://www.asasrms.org/Proceedings/papers/2000_099.pdf
- Parker JD, Talih M, Malec DJ, et al. National Center for Health Statistics data presentation standards for proportions. Vital Health Stat 2 2017; 175:1–22. PMID:30248016
- Yue X, Black CL, Ball S, et al. Workplace interventions associated with influenza vaccination coverage among health care personnel in ambulatory care settings during the 2013-2014 and 2014-2015 influenza seasons. Am J Infection Control 2017;45:1243-1248.
- Dooling K, McClung N, Chamberland M, et al. The Advisory Committee on Immunization Practices' Interim Recommendation for Allocating Initial Supplies of COVID-19 Vaccine — United States, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1857-1859. DOI: http://dx.doi.org/10.15585/wwmr.mm6949e1
- Dey P, Halder S, Collins S, Benons L, Woodman C. Promoting uptake of influenza vaccination among healthcare workers: A randomized controlled trial. J Pub Health Med 2001;23: 346-348.
- McMichael TM, Clark S, Pogosjans S, et al. COVID-19 in a long-term care facility — King County, Washington, February 27–March 9, 2020. MMWR Morb Mortal Wkly Rep 2020;69:339-342
- Schropp S, Calhoun, K, Razzaghi H, Black, CL. Concerns about bivalent COVID-19 vaccine and reasons for non-vaccination among adults who completed a primary series – Omnibus survey, March 10–April 30, 2023 & Household Pulse Survey, March 1–April 10, 2023. Atlanta, GA: US Department of Health and Human Services, CDC; https://www.cdc.gov/vaccines/imz-managers/coverage/covidvaxview/pubs-resources/covid-vaccine-reasons-non-vaccination.html
- Ferdinands JM, Rao S, Dixon BE, et al. Waning 2-Dose and 3-Dose Effectiveness of mRNA Vaccines Against COVID-19—Associated Emergency Department and Urgent Care Encounters and Hospitalizations Among Adults During Periods of Delta and Omicron Variant Predominance — VISION Network, 10 States, August 2021—January 2022. MMWR Morb Mortal Wkly Rep 2022;71:255-263. DOI: http://dx.doi.org/10.15585/mmwr.mm7107e2.
- Community Preventive Services Task Force. Worksite: seasonal influenza vaccinations using interventions with on-site, free, actively promoted vaccinations—healthcare workers. Atlanta, GA: US Department of Health and Human Services, CDC, Community Preventive Services Task Force; 2021. https://www.thecommunityguide.org/findings/worksite-seasonal-influenza-vaccinations-healthcare-on-site
- CDC. Post-acute and Long-term Care Facility Toolkit: Influenza Vaccination among Healthcare Personnel Atlanta, GA: US Department of Health and Human Services, CDC; 2020. Accessed September 6, 2022. Long-term-care-toolkit.pdf (cdc.gov)
