What to know
This algorithm is intended to assist in the interpretation of influenza testing results and clinical decision-making during periods (e.g. during summer months) when influenza viruses are NOT circulating in the community
Algorithm
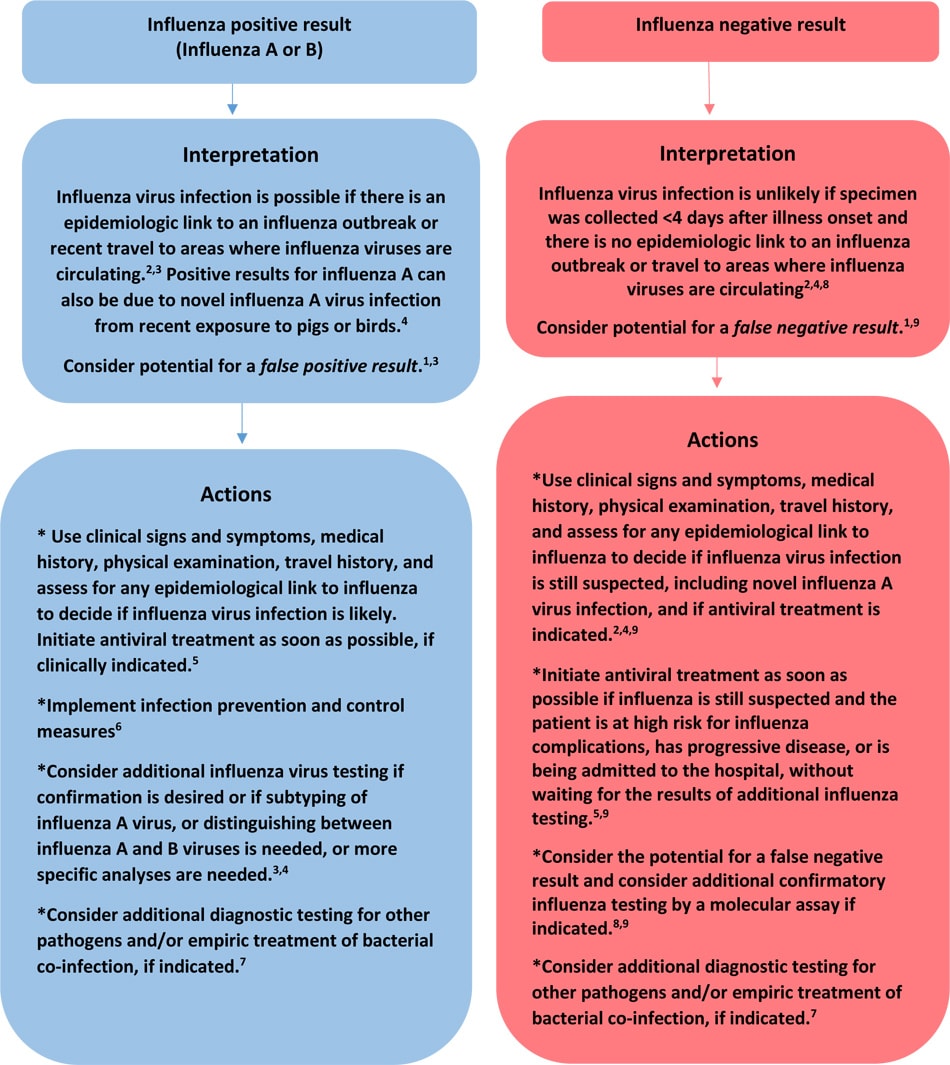
1.During periods when influenza activity is low and there is low influenza virus circulation among persons in the community, the positive predictive value of influenza tests is low (that is, the chance that a positive result indicates that the patient has influenza is low – consider potential for a false positive result), and the negative predictive value is high (the chance that a negative result indicates that the patient does not have influenza is high – likely true negative result ). Even though most influenza tests have high specificity, false positive results are more common when influenza activity is low. During periods when influenza viruses are not circulating in the community, confirmation of positive results of antigen detection assays (rapid influenza diagnostic test or immunofluorescence assay) should be considered by RT-PCR or other molecular assays, and the local or state health department should be consulted.
2. It is important to ascertain if the patient has an epidemiological link to someone with known influenza, (i.e., known influenza virus exposure). Is the patient linked to an influenza outbreak (e.g., institutional outbreak, organized group tour outbreak – cruise ship/bus/train, summer camp outbreak) or has the patient or any sick contacts had recent travel to an area where influenza viruses are circulating (e.g., temperate climate countries in the Southern Hemisphere, tropical or subtropical climate countries)?
3.Influenza virus infection may include seasonal influenza A (H3N2), A(H1N1)pdm09, influenza B, or rarely, novel influenza A virus infection. The interpretation of a positive influenza testing result will, in part, depend on the test used – some tests only detect influenza A virus, some will detect influenza B virus, and some will detect both A and B viruses. If tests for both influenza A and influenza B are positive, refer specimen to a public health laboratory for resolution, as dual infections are uncommon.
4. Most available tests do not distinguish between influenza A virus subtypes, and cannot distinguish between seasonal influenza A viruses and novel influenza A viruses, and may not detect all novel influenza A viruses. If subtyping is needed, specimens should be sent to a state public health laboratory. If there has been recent exposure to pigs or birds (poultry or wild birds) or other animals (e.g., dairy cows) or to a sick person with confirmed or suspected novel influenza A virus infection, the state health department should be notified immediately, and specimens should be forwarded for RT-PCR at a public health laboratory (e.g., state health department virology laboratory). Note that recommended infection and prevention control measures should be followed when collecting respiratory specimens, including from patients with suspected novel influenza A virus infection.
5. Antiviral treatment is recommended as soon as possible for all of the following who have suspected or confirmed influenza: outpatients who are at high-risk for influenza complications, persons with severe or progressive disease, and all hospitalized patients.
6. Prevention Strategies for Seasonal Influenza in Healthcare Settings
7. Consult the local or state health department or other sources (e.g., virology testing at a local hospital) for local activity on other respiratory pathogens associated with acute respiratory illness. Empiric antibiotic coverage for possible secondary bacterial infections should include coverage for Streptococcus pneumoniae, Staphylococcus aureus (including MRSA), and Group A Streptococcus, especially for hospitalized adult patients (see the Infectious Diseases Society of America (IDSA)/American Thoracic Society (ATS) Community-acquired Pneumonia guidelines) and for some children (see the Pediatric Infectious Diseases Society of America (PIDS)/Infectious Diseases Society of America (IDSA) Community-acquired Pneumonia guidelines).
8. Respiratory specimens should be collected as close to illness onset as possible to maximize detection of influenza viruses. Influenza viral shedding in the upper respiratory tract declines after about 3-4 days in most people. Infants, young children, immunocompromised patients can shed influenza viruses for longer duration. Molecular assays can detect influenza viral RNA for longer periods than antigen detection assays. If the patient is critically ill on invasive mechanical ventilation, and has tested negative for influenza viruses on an upper respiratory tract specimen, including by a molecular assay, then a lower respiratory tract specimen (endotracheal aspirate or bronchioalveolar lavage fluid) should be collected for influenza testing by RT-PCR or other molecular assays.
9. If the influenza test used is an antigen detection assay (rapid influenza diagnostic test or immunofluorescence assay) that has suboptimal sensitivity to detect influenza virus in respiratory specimens compared to a "gold standard test" such as RT-PCR or viral culture, a negative result does not exclude influenza virus infection and could be a false negative result, especially if a history of exposure to influenza viruses is identified and the patient has signs and symptoms or complications consistent with influenza. If influenza is still suspected, confirmation of a negative result of an antigen detection assay by RT-PCR or other molecular assays should be considered, and the local or state health department should be consulted. Do not use negative results of antigen detection assays exclusively for clinical decision-making, or for public health decisions, including identifying influenza outbreaks, or for decisions on implementation of infection prevention and control measures. The Infectious Diseases Society of America (IDSA) recommends use of rapid influenza molecular assays over rapid influenza diagnostic tests (RIDTs) for detection of influenza viruses in respiratory specimens of outpatients. IDSA recommends use of RT-PCR or other molecular assays for detection of influenza viruses in respiratory specimens of hospitalized patients.
