Key points
- A disproportionate number of antimicrobial-resistant infections negatively impact people who are at higher risk for health disparities and inequities.
- Disparities in antimicrobial-resistant threats exist across all social determinants of health, including health care, the food supply and the community.
- CDC is prioritizing health disparities/inequality related to antimicrobial resistance through programs like Project Firstline, Antimicrobial Resistance Laboratory Network and National Healthcare Safety Network.
CDC prioritizes health equity issues across AR
Posted: March 2022
More than 2.8 million antimicrobial-resistant infections occur in the U.S. each year, and more than 35,000 people die as a result. When Clostridioides difficile—a bacterium (germ) that is not typically resistant but can cause deadly diarrhea and is associated with antibiotic use—is added to these, the U.S. toll exceeds 3 million infections and 48,000 deaths. A disproportionate number of resistant infections negatively impacts people who are at higher risk for health disparities and inequities.
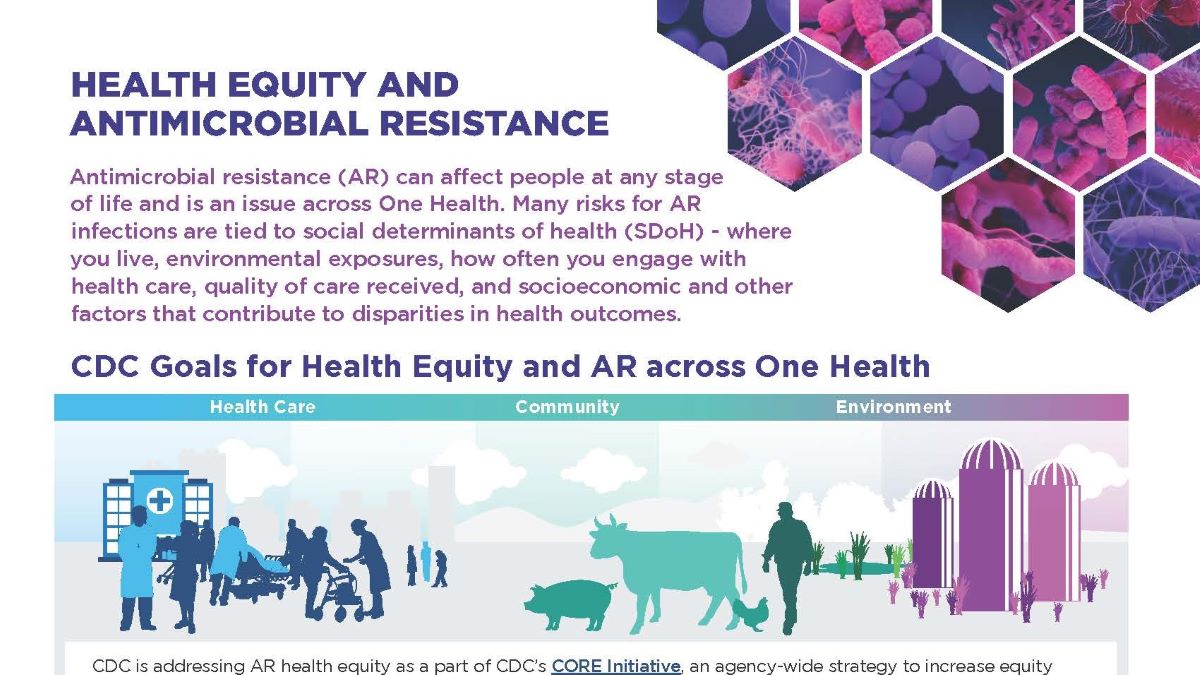
Many risks for antimicrobial-resistant infections are tied to the social determinants of health (SDoH)—conditions in the places where people live, learn, work and play that affect a wide range of health outcomes and quality of life. Identifying and addressing these impacts is vital for improving health outcomes and reducing the burden of AR. Antimicrobial-resistant threats cause health disparities across age, race and gender in settings spanning a One Health spectrum—in health care, the food supply, the environment and the community.
- Data on healthcare-associated infections (HAIs) show disparities particularly among people of color, pregnant women, older adults and people with weakened immune systems or certain medical conditions, such as diabetes.
- Antimicrobial-resistant infections disproportionately impact young children, men who have sex with men (MSM) and groups that have historically experienced greater obstacles based on their racial or ethnic group.
- Disparities related to antimicrobial resistance are impacted by structural inequities and socioeconomic factors such as household income, type of housing (crowding, persons experiencing homelessness), immigration, type of health insurance, access to health care and education level.
- Geography and the built environment (buildings, neighborhoods, parks, roads) also play a role in health disparities related to antimicrobial resistance, leading to higher rates of infection among people experiencing homelessness or people facing housing insecurity, travelers to countries with unsafe water and inadequate sanitation and people living in certain metropolitan cities.
We know that more research and action is needed to fully understand potential disparities related to antimicrobial resistance and this is a priority for CDC. CDC is working across programs to understand disparities and improve health equity, including through:
- Project Firstline to address training gaps for healthcare workers from diverse educational and training backgrounds.
- The Antimicrobial Resistance Laboratory Network to analyze patient demographic data alongside laboratory test results to provide a more comprehensive picture of antimicrobial resistance in certain populations.
- The National Healthcare Safety Network to provide patient demographic data for future analysis and drive improvement in health care quality.
Through this work and more, CDC is addressing antimicrobial resistance and health equity as part of CDC's CORE Initiative, an agency-wide strategy to increase equity across public health.
