Key points
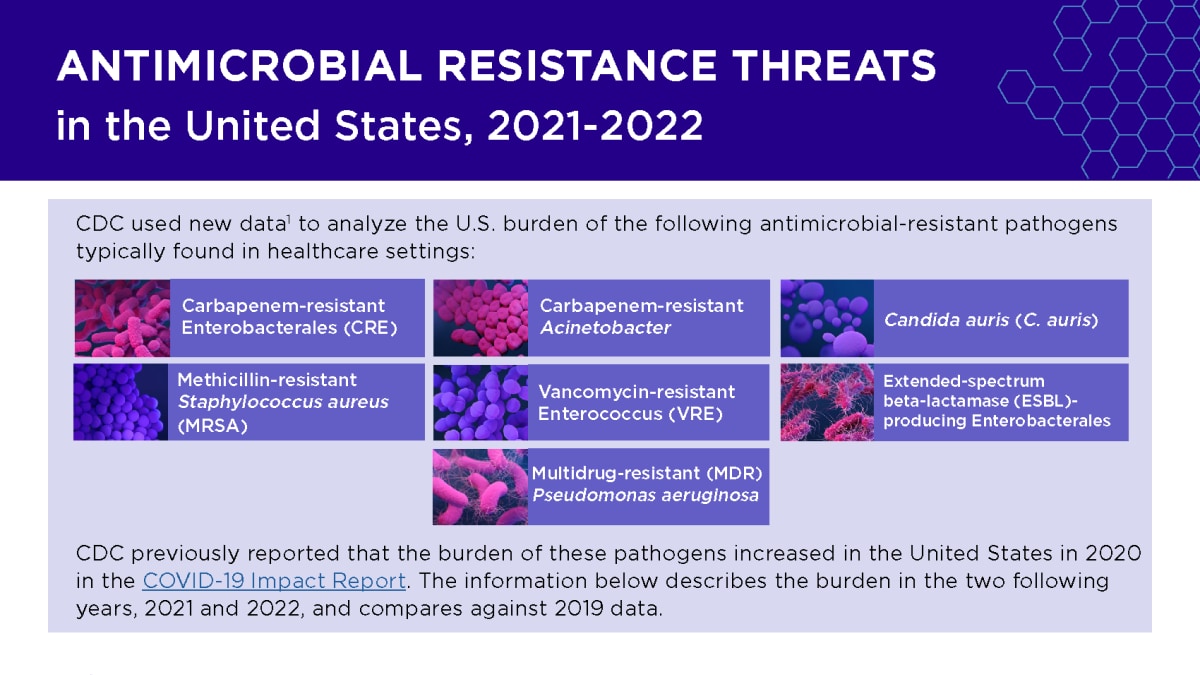
- CDC used new data to update the United States (U.S.) burden of seven antimicrobial-resistant pathogens typically found in healthcare settings.
- CDC previously reported that the burden of these pathogens increased in the U.S. in 2020 in the COVID-19 Impact Report.
- The new data describe the burden in the two following years, 2021 and 2022, and compares against 2019 data.
Findings
In July 2024, CDC published a fact sheet using new dataA to update the U.S. burden of the following seven antimicrobial-resistant pathogens typically found in healthcare settings:
- Carbapenem-resistant Enterobacterales (CRE)
- Carbapenem-resistant Acinetobacter
- Candida auris (C. auris)
- Methicillin-resistant Staphylococcus aureus (MRSA)
- Vancomycin-resistant Enterococcus (VRE)
- Extended-spectrum beta-lactamase (ESBL)-producing Enterobacterales
- Multidrug-resistant (MDR) Pseudomonas aeruginosa
CDC previously reported that the burden of these pathogens increased in the U.S. in 2020 in the COVID-19 Impact Report. The new data describe the burden in the two following years, 2021 and 2022, and compares against 2019 data.
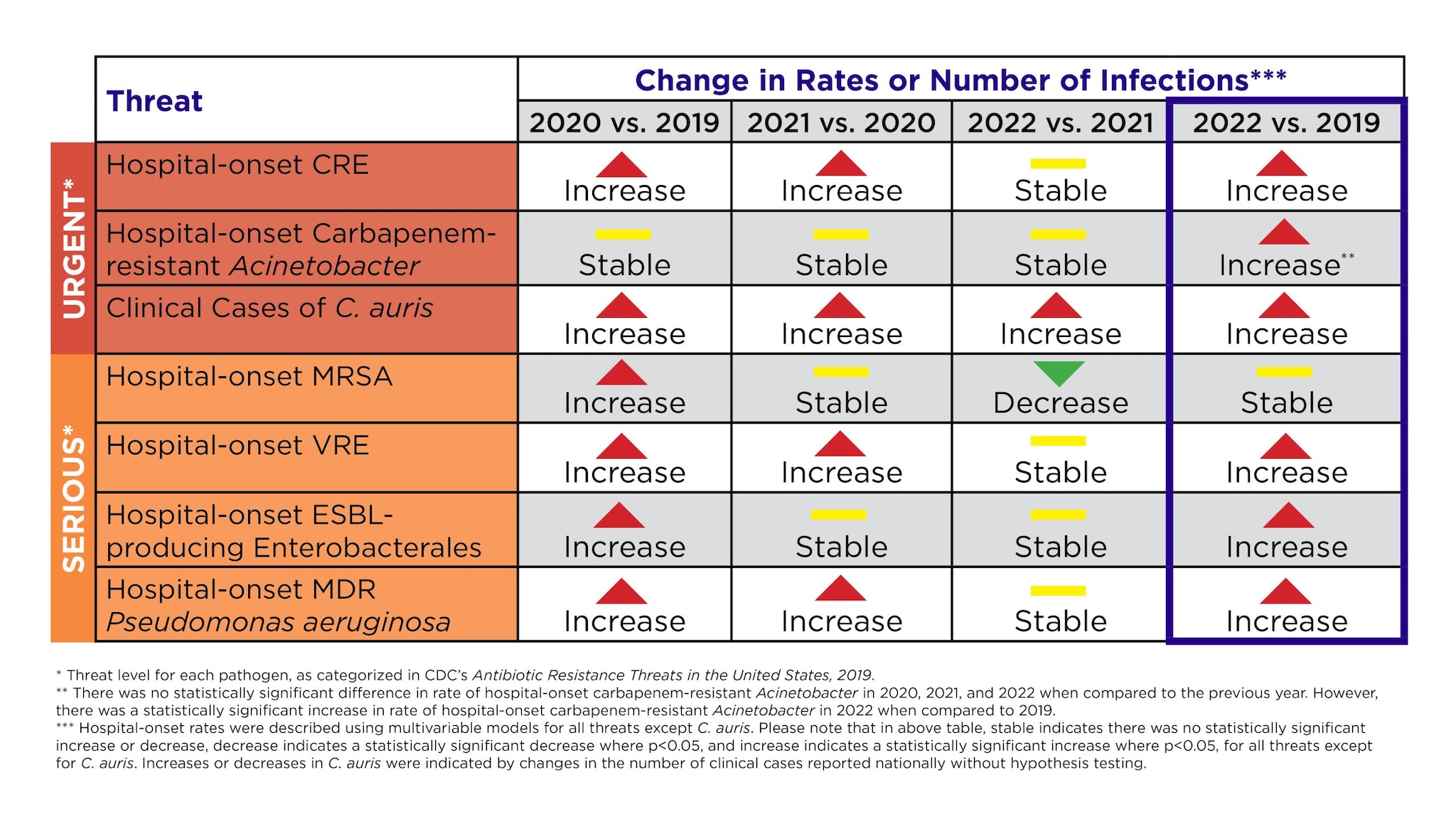
The new dataA show that six bacterial antimicrobial-resistant hospital-onset infectionsB increased by a combined 20% during the COVID-19 pandemic compared to the pre-pandemic period, peaking in 2021, and remaining above pre-pandemic levels in 2022. In 2022, rates for all but one of these pathogens (MRSA) remained above pre-pandemic levels. In addition, the number of reported clinical cases of C. auris—a type of yeast that can spread in healthcare facilities, is often resistant to antifungal medications, and can cause severe illness—increased nearly five-fold from 2019 to 2022.
Impacts of COVID-19 on antimicrobial resistance
The increases in antimicrobial resistance (AR) burden seen in 2020 and 2021 are likely due in part to the impact of COVID-19, which pushed healthcare facilities, health departments and communities near their breaking points. The pandemic resulted in longer hospital stays for hospitalized patients (including those diagnosed with COVID-19), challenged the implementation of infection prevention and control practices and increased inappropriate antibiotic use.
As the pandemic continued, healthcare providers and public health professionals took aggressive action to prevent infections and protect lives, helping to reduce the burden of AR from its 2021 peak. CDC supported many of these efforts through American Rescue Plan Act (ARP) funding to health-department Healthcare-Associated Infections and Antimicrobial Resistance (HAI/AR) Programs and CDC’s Antimicrobial Resistance Laboratory Network (AR Lab Network) in all U.S. states, as well as some large cities and territories.
Actions against antimicrobial resistance
In the first year of work supported by ARP funding, health departments invested in proven strategies and initiatives including:
- More than 9,000 prevention-based infection control assessments in healthcare facilities.
- More than 5,300 outbreak responses to novel multidrug-resistant germs.
- More than 90,000 healthcare workers trained in infection prevention and control.B
In 2021 and 2022, CDC’s AR Lab Network tested more than 230,000 patient samples for detection and characterization of antimicrobial-resistant organisms. This testing helped inform efforts to stop spread and protect patients.
Additional action is critical
The future of CDC AR threats reporting

CDC's previous antimicrobial resistance threats reports, published in 2013 and 2019, were important resources to guide U.S. policy for and investments in combating antimicrobial resistance.
Starting in 2025, CDC will release estimates for at least 19 antimicrobial resistance threats and an update on the U.S. burden of antimicrobial resistance, by pathogen, in a new electronic format.
Going forward, CDC will release new estimates for the burden of these threats at least every two years. Data are critical to guide efforts to combat antimicrobial resistance, and CDC is committed to providing the high-quality data required to steer this important work.
Resources
Web pages
Factsheet
- Databases used for bacterial pathogens analyzed were the PINC-AI Healthcare Database and the BD Insights Research Database. CDC is working on a future publication that will include more detailed data analysis for bacterial pathogens discussed in this fact sheet. C. auris data was obtained by monthly reporting through jurisdiction public health departments.
- Data shown reflect activities from the first year of ARP supplements, October 2021-August 2022.