At a glance
Adults are at risk of illness, hospitalization, disability, and, in some cases, death from vaccine-preventable diseases, particularly influenza (flu) and pneumococcal disease. Many adults in the United States have not received recommended vaccinations and racial/ethnic vaccination differences persist.
Summary
Adults are at risk of illness, hospitalization, disability and even death from vaccine-preventable diseases, particularly influenza and pneumococcal disease. The Centers for Disease Control and Prevention (CDC) recommends vaccinations for adults based on age, health conditions, prior vaccination history, and other factors12to prevent vaccine-preventable diseases and related outcomes. A composite immunization quality measure was recently developed to track influenza, pneumococcal, herpes zoster, and tetanus and diphtheria toxoids (Td) or tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) vaccination among adults3. This report summarizes data on vaccination coverage for U.S. adults aged >19 years using data from the 2016 and 2017 National Health Interview Survey (NHIS), an in-person survey of eligible civilian non-institutionalized adults4. Estimates for the adult composite measure and its component vaccines are presented below; coverage data for other recommended adult vaccines are included in supplementary material linked at the bottom of this page.
Compared with 2016 NHIS estimates, influenza vaccination among adults aged ≥19 years increased to 45.4% (+1.9 percentage points) and Tdap vaccination increased to 31.7% (+5.1 percentage points). Coverage for the adult age-appropriate composite measures including influenza and any tetanus vaccine was low in all age groups, ranging from 14.5% in adults aged 60-64 years to 26.7% in adults aged 19-59 years. Racial and ethnic differences in vaccination coverage persisted for all vaccinations in this report with lower coverage for most vaccinations among non-white compared with white adults. Interpretation of these results should take into account limitations of the survey, including reliance on self-report of vaccination status and decreasing response rates. Because of these limitations, CDC is examining other potential data sources to assess utilization of adult vaccination. However, the NHIS data indicate that many adults remain unprotected against vaccine-preventable diseases. Substantial improvement in adult vaccination uptake is needed to maximally reduce the impact of vaccine-preventable diseases. Following the Standards for Adult Immunization Practice all providers should routinely assess adults’ vaccination status at every clinical encounter, strongly recommend needed vaccines, either offer needed vaccines or refer their patients to another provider who can administer the recommended vaccine, and document vaccinations received by their patients in an immunization information system (IIS).
Methods
NHIS collects information about the health and health care of the noninstitutionalized U.S. civilian population using nationally representative samples4. Face-to-face interviews are conducted by the U.S. Census Bureau for CDC’s National Center for Health Statistics. Non-institutionalized adults aged >19 years with interviews conducted during August 2016-June 2017 (for influenza vaccination) and January–December 2017 (for pneumococcal, Td, Tdap, hepatitis A, hepatitis B, herpes zoster, and HPV vaccination) were included in this analysis. The total adult sample was 26,430 persons aged ≥19 years. The final sample adult component response rate was 54.3% for the 2016 NHIS and 53.0% for the 2017 NHIS. NHIS methods have been previously published. Questions about receipt of vaccinations recommended for adults are asked of one randomly selected adult within each family in the household. Weighted data were used to produce national vaccination coverage estimates. For non-influenza adult vaccination coverage estimates, the weighted proportion of respondents who reported receiving selected vaccinations was calculated. To better assess influenza vaccination coverage for the 2016-17 season, the Kaplan-Meier survival analysis procedure was used. Race/ethnicity was categorized as follows: white, black, Hispanic, Asian and “other.” In this report, persons identified as white, black, Asian, or other race are non-Hispanic. Persons identified as Hispanic might be of any race. “Other” includes American Indian/Alaska Native and persons who identified multiple races. The five racial/ethnic categories are mutually exclusive. For the adult vaccination composite measure, data from the 2017 NHIS were analyzed to determine estimates for a composite measure of vaccination coverage for select vaccines routinely recommended for all adults aged ≥19 years (Td, Tdap, and influenza vaccine) or indicated based on age (herpes zoster and pneumococcal vaccines) and three age groups (age 19–59 years, age 60–64 years, and age ≥65 years) based on the vaccines recommended for that age group. Estimates for composite measures were calculated to include Tdap vaccine in the past 10 years (Method 1) or any tetanus-toxoid containing vaccine in the past 10 years (Method 2), and both with and without influenza vaccination in the past 12 months. Point estimates and 95% confidence intervals (CIs) were calculated by using SUDAAN software (Research Triangle Institute, Research Triangle Park, NC, version 11.0.1) to account for the complex sample design. T-tests were used for comparisons between data years and for comparisons of each level of each respondent characteristic to a chosen referent level (e.g., for race/ethnicity, white was the reference group). Statistical significance was defined as p<0.05. Coverage estimates are not reported for small sample size (n<30) or inflated relative standard error (standard error/estimates >0.3).
Results
- Influenza vaccination coverage for the 2016-17 season among adults aged >19 years was 45.4%, a 1.9 percentage points increase from the 2015-2016 season.
- In the 2016-17 season, coverage among white adults aged >19 years (48.2%) was higher than that for black (38.5%) and Hispanic adults (37.0%).
- Influenza vaccination coverage among adults aged >19 years with high-risk conditions was 59.7% in the 2016-17 season, similar to estimates for the 2015-16 season.
- Among adults aged >19 years with high-risk conditions, coverage was higher among white adults (61.4%) than Hispanic adults (52.0%).
- Pneumococcal vaccination coverage among adults aged 19-64 years at increased risk for pneumococcal disease was 24.5% in 2017, similar to the estimate for 2016.
- Pneumococcal vaccination coverage among adults aged >65 years was 69.0% in 2017, similar to the estimate for 2016.
- Pneumococcal vaccination coverage among white adults aged >65 years was higher than that for adults of other racial/ethnic groups.
- Herpes zoster vaccination coverage was 34.9% among all adults aged >60 years, similar to the estimate for 2016.
- Compared with the estimates for 2016, herpes zoster vaccination coverage increased 10.0 percentage points among Asian adults but remained stable in all other racial/ethnic groups.
- White adults aged >60 years had higher herpes zoster vaccination coverage compared with adults of all other racial/ethnic groups.
- In 2017, the proportion of adults aged >19 years reporting having received any tetanus toxoid-containing vaccination during the past 10 years was 63.4%, similar to estimates for 2016.
- Among adults aged >19 years for whom Tdap vaccination could be assessed, Tdap vaccination in the past ten years increased from 2016 to 2017 overall and by age group.
- Among adults aged ≥19 years, white adults had higher coverage compared with black, Hispanic, and Asian adults for any tetanus vaccine and for Tdap vaccination.
- In 2017, a composite measure consisting of routinely recommended age-appropriate vaccines was developed (including tetanus vaccination, herpes zoster, and pneumococcal vaccination, with or without influenza vaccination).
- In 2017, few adults aged ≥19 years had received all age-appropriate vaccines included in the composite measure regardless of whether Tdap (Method 1) or any tetanus-containing vaccine (Method 2) was measured.
- Adults aged 60-64 years had the lowest composite vaccination coverage using either method of measurement. Low coverage with herpes zoster vaccine is the primary driver of this result.
From 2010-2017, although point estimates for each year generally varied by only a few percentage points, linear trend tests indicated coverage increases for most vaccines in this report (see: Box 1/Figure 1, Box 2/Figure 1, Box 3/Figure 1 for additional estimates). Average annual increases ranged from 0.8 percentage points for pneumococcal vaccination among persons aged 19-64 years at increased risk of disease to 3.3 percentage points for Tdap among adults aged >19 years.
FIGURE 1. Estimated proportion of adults aged ≥19 years who received selected vaccines, *by age group and risk status — National Health Interview Survey, United States, 2010–2017. See data file
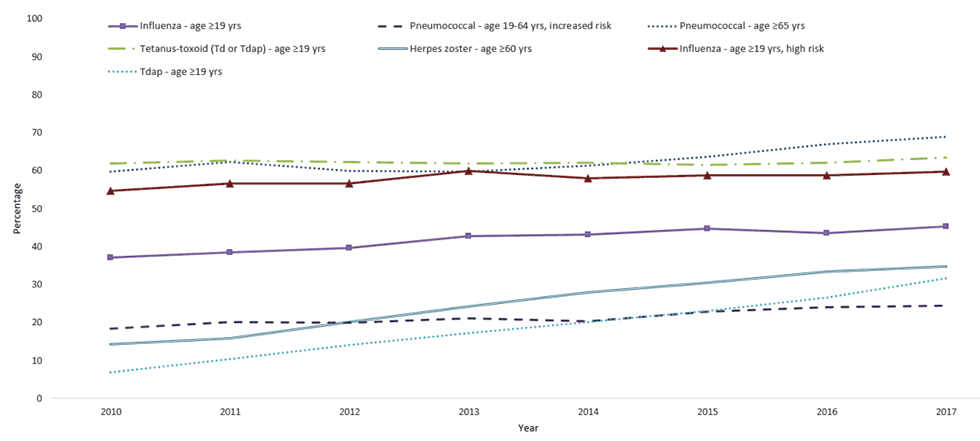
Abbreviations: Td = tetanus and diphtheria toxoids; Tdap = tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine.
*Tdap vaccination coverage data among adults aged ≥65 years are available beginning in the NHIS 2012 survey.
- Vaccination coverage for selected vaccinations was estimated for adults aged >19 years who were healthcare personnel (See: Box 1).
- Hepatitis A and hepatitis B vaccination among persons aged >19 years overall, by age group, race/ethnicity and among select populations (See: Box 2).
- Human papillomavirus vaccination, by age group, sex, and race/ethnicity (See: Box 3).
- Differences in vaccination coverage among adults aged ≥19 years for select vaccines, by race/ethnicity, age group, increased-risk status, health insurance status, access to care characteristics, nativity, number of years living in the United States, and citizenship (See: Box 4)
BOX 1: HCP Tables. Vaccination coverage among health care personnel (HCP) aged >19 years for selected vaccines — National Health Interview Survey, United States, 2017*
| Supplementary Table | URL (hyperlinked) | Result summary |
|---|---|---|
| Proportion of Health Care Personnel Who Received Selected Vaccinations | Box 1/ Table 1 [1 sheet] Table 1 HCP |
Overall, in 2017, influenza and tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) vaccination coverage increased among HCP aged >19 years (5.2 and 8.5 percentage points, respectively) compared with 2016 estimates. Hepatitis B vaccination coverage for 2017 among HCP aged >19 years was similar to 2016 estimates. White HCP had higher vaccination coverage compared with black HCP (influenza, Tdap, and hepatitis B vaccination) and Hispanic HCP (hepatitis B vaccination). Asian HCP had higher hepatitis B vaccination coverage compared with white HCP. |
| Proportion of Health Care Personnel with Direct Patient Care Who Received Selected Vaccinations | Box 1/ Table 2 [1 sheet] Table 2 HCP Direct Contact |
Overall, in 2017, influenza vaccination coverage increased 7.1 percentage points to 68.1% among HCP ≥19 years without direct patient care, compared with the estimate for 2016. Tdap vaccination coverage among HCP ≥19 years with direct patient care increased 8.6 percentage points to 61.8% compared with the estimate for 2016. Tdap and hepatitis B vaccination coverage was higher among HCP with direct patient care compared with those without direct patient care. |
| Proportion of Adults Who Received Tdap Among Those Reporting Tetanus Vaccination by Health Care Personnel Status | Box 1/ Table 3 [1 sheet] Table 3 Tdap type |
Among adults >19 years, 41.9% reported they knew what type of tetanus vaccine they received, 42.8% reported they were not informed of the vaccination type, and 15.4% could not recall the type of tetanus vaccination received. Among those who reported they knew what type tetanus vaccine they received, 75.2% reported receiving Tdap. HCP reported receipt of Tdap more often than did non-HCP. |
*Detailed information from these analyses are shown in Box1_HCP /Tables 1-3 available at: AltText _Box1_HCP [2 pages].
BOX 2: Hep A B Tables. Estimated proportion of adults ≥19 years who received hepatitis A and hepatitis B vaccines, by age group, increased-risk status, and race/ethnicity — National Health Interview Survey, United States, 2017*
| Supplementary Table | URL (hyperlinked) | Result summary |
|---|---|---|
| Proportion of Adults ≥19 Years Who Received Hepatitis A Vaccination by Age Group, Increased-risk Status, and Race/ethnicity | Box 2/ Table 1 [1 sheet] Table 1 Hep A |
In 2017, reported hepatitis A vaccination coverage (>2 doses) was 10.9% for adults >19 years, and 6.1% for adults >50 years, similar to the estimates for 2016, while coverage among adults 19-49 years was 15.7% in 2017, a 2.3 percentage points increase compared with 2016.
Among adults 19-49 years, compared with whites (16.3%), coverage was lower for blacks (11.7%) and Hispanics (13.4%), while coverage was higher for Asians (23.3%). Among adults >19, 19-49, and ≥50 years, vaccination coverage was higher among adults who had traveled outside the United States to a country in which hepatitis A is of high or intermediate endemicity than among respondents who did not travel outside the United States or had traveled only to countries in which the disease is of low endemicity. Hepatitis A vaccination coverage among adults >19 and >50 years with chronic liver conditions was 20.8% and 19.2%, a 7.9 percentage points and 10.0 percentage points increase compared with the 2016 estimates, respectively. |
| Proportion of Adults ≥19 Years Who Received Hepatitis B Vaccination by Age Group, Increased-risk Status, and Race/ethnicity | Box 2/ Table 2 [1 sheet] Table 2 Hep B |
In 2017, reported hepatitis B vaccination coverage (>3 doses) was 25.8% for adults >19 years, 34.3% for adults 19-49 years, and 16.6% for adults >50 years, similar to the estimates for 2016.
Among adults 19-49 years, coverage for blacks (30.7%) and Hispanics (27.3%) was lower than that for whites (36.6%). Among adults >19, 19-49, and ≥50 years, vaccination coverage was higher among adults who had traveled outside the United States to a country in which hepatitis B is of high or intermediate endemicity than among respondents who did not travel outside the United States or had traveled only to countries in which the disease is of low endemicity. |
*Detailed information from these analyses are shown in Box 2_Hep A_B/ Tables 1-2 available at: AltText_Box2_HepA_B [3 pages].
BOX 3: HPV Tables. Estimated proportion of adults ≥19 years who received human papillomavirus (HPV) vaccination, by age group, sex, and race/ethnicity — National Health Interview Survey, United States, 2017*
| Supplementary Table | URL (hyperlinked) | Result summary |
|---|---|---|
| Age at First Dose of HPV Vaccination | Box 3/ Table 1 [1 sheet] Table1 HPV Age at 1st dose |
Among females 19-26 years, 2.7% reported receiving the first dose of HPV vaccine at 8-10 years, 13.5% reported receiving the first dose of HPV vaccine at 11-12 years, 66.7% at 13-17 years, 6.7% at 18 years, and 10.4% at 19-26 years. Among males 19-26 years, 8.3% reported receiving the first dose of HPV vaccine at 8-10 years, 3.7% at 11-12 years, 42.1% at 13-17 years, 16.6% at 18 years, and 29.3% at 19-26 years. Among respondents 19–26 years, the difference between the age reported at the time of the interview and the age at which respondents indicated that the first dose of HPV vaccine was received was ≥13 years for 4.4% of females and for 3.6% of males. This would imply receipt of vaccination in 2004 or earlier, before HPV vaccine was licensed for use in 2006. |
| Proportion of Adults 19-26 Years Who Received HPV Vaccination | Box 3/ Table 2 [1 sheet] Table 2 HPV |
In 2017, among females 19-26 years, 51.5% reported receipt of at least one dose of HPV vaccine, similar to the estimates for 2016. Hispanics (38.8%) had lower coverage compared with whites (57.4%).
Among females 19-21 years, HPV vaccination coverage was 51.8%, similar to the estimate for 2016. Among females 22-26 years, HPV vaccination coverage was 51.3%, similar to the 2016 estimate. Among males 19-26 years, 19-21 years and 22-26 years, HPV vaccination coverage (at least one doses) was 21.2%, 33.7% and 15.1%, increases of 7.6, 12.4 and 5.9 percentage points, respectively. HPV vaccination (at least one dose) among females 19-26 years who had not received HPV vaccination prior to age 19 years was 8.6%, similar to the estimate for 2016. Among males 19-26 years who had not received HPV vaccination prior to age 19 years, HPV vaccination was 5.8%, a 3.1 percentage points increase compared with the estimate reported for 2016. |
*Detailed information from these analyses are shown in Box 3_HPV/ Tables 1-2 available at: AltText_Box3_HPV [2 pages].
BOX 4: Disparities Tables.Differences in vaccination coverage among adults aged ≥19 years for select vaccines, by race/ethnicity, age group, increased-risk status, health insurance status, access to care characteristics, nativity, number of years living in the United States, and citizenship — National Health Interview Survey, United States, 2017*
| Supplementary Table | URL (hyperlinked) | Result summary |
|---|---|---|
| Racial/Ethnic Differences in Vaccination Coverage Among Adults | Box 4/ Table 1 [1 sheet] Table 1 Summary R/E diff |
Compared with 2016, racial/ethnic differences in vaccination coverage persisted for all seven vaccines in this report. With whites as the reference group, there were differences in vaccination coverage for 49 of the 66 comparisons by vaccine and age/target groups (not including comparisons of the “other” race/ethnic group). |
| Average Change in Racial/Ethnic Vaccination Coverage Differences Among Adults, 2010–2017 | Box 4/ Table 2 [1 sheet] Table 2 Avg change R/E diff |
During 2010–2017, vaccination differences between whites and blacks increased for tetanus vaccination (Td or Tdap) (adults ≥19 years and 19-49 years), Tdap (all age groups), hepatitis A (adults 19-49 years), hepatitis B (adults 19-49 years), and herpes zoster vaccination (adults ≥60 years and ≥65 years). Among Hispanics, vaccination differences increased over this time period compared with whites for tetanus vaccination (Td or Tdap) (adults ≥19 years), Tdap (all age groups and HCP≥19 years), hepatitis A (adults 19-49 years), and herpes zoster vaccination (adults ≥60 years and ≥65 years). For Asians, vaccination differences increased over this time period compared with whites for Tdap (adults 19-64 years), and herpes zoster vaccination (adults >65 years). |
| Proportion of Adult Who Received Influenza Vaccination By Age And Race/Ethnicity | Box 4/ Table 3 [1 sheet] Table 3 Flu |
Influenza vaccination coverage for the 2016-17 season overall among adults >19 years was 45.4%, a 1.9 percentage points increase from the 2015-2016 season. Coverage among whites ≥19 years (48.2%) was higher than that for blacks (38.5%) and Hispanics (37.0%). Among adults 19-49 years, influenza vaccination coverage for the 2016–17 season overall increased by 2.4 percentage points to 34.5% compared with the 2015–16 season estimate. In the 2016-17 season, coverage among whites 19-49 years (35.3%) was higher than that for blacks (29.6%); coverage for whites was lower than that for Asians (42.6%). Coverage among whites 50-64 years (48.8%) was higher compared with blacks (41.8%) and Hispanics (40.0%). Coverage among whites ≥65 years (72.4%) was higher compared with blacks (64.4%). |
| Proportion of Adult Who Received Tetanus Vaccination, and Tetanus Vaccination Including Pertussis Vaccine By Age And Race/Ethnicity | Box 4/ Table 4 [1 sheet] Table 4 Tetanus |
In 2017, whites had higher tetanus vaccination (Td or Tdap) coverage across all age groups compared with blacks, Hispanics, and Asians. Whites had higher Tdap vaccination coverage across all age groups compared with blacks and Hispanics, and higher coverage compared with Asians among adults ≥19 years and 19-64 years. |
| Proportion of Adult Who Received Herpes Zoster Vaccination By Age And Race/Ethnicity | Box 4/ Table 5 [1 sheet] Table 5 Herpes |
Among adults 60-64 years, 22.4% reported herpes zoster vaccination, similar to the estimate for 2016. Whites 60-64 years had higher herpes vaccination coverage (24.8%) compared with blacks (12.7%), and Hispanics (17.3%). Among adults ≥65 years, 40.2% reported herpes zoster vaccination, similar to the estimates for 2016. Whites ≥65 years had higher herpes zoster vaccination coverage (45.0%) compared with blacks (19.4%), Hispanics (21.4%), Asians (36.8%), and adults indicating other race/ethnicity (31.3%). The difference in vaccination coverage between whites and other racial/ethnic groups in 2017 increased only for respondents ≥65 years indicating other race/ethnicity and decreased only for Asians ≥65 years compared with differences measured in 2016. |
| Association of Health Insurance Status with Vaccination Coverage Among Adult Populations | Box 4/ Table 6 [1 sheet] Table 6 Insurance overall |
Overall, vaccination coverage was generally lower among adults without health insurance compared with those with health insurance. Adult vaccination coverage differed by the type of health insurance. Generally, with the exception of influenza vaccination and pneumococcal vaccination, vaccination coverage was higher among adults with private health insurance compared with those reporting public health insurance. |
| Association of Health Insurance Status and Having a Usual Place for Health Care with Vaccination Coverage | Box 4/ Table 7 [1 sheet] Table 7 Ins-physician |
Generally, adults with a usual place for health care were more likely to report having received recommended vaccinations than those who did not have a usual place for health care, regardless of whether they had health insurance. Among adults with health insurance, coverage was higher among those who reported having a usual place for health care compared with those who did not have a usual place for health care. |
| Adult Vaccination Coverage by Health Insurance Status and Physician Contacts | Box 4/ Table 8 [1 sheet] Table 8 Ins-contacts |
Generally, vaccination coverage was higher among those reporting having had one or more physician contacts in the past year compared with those who had not visited a physician in the past year, regardless of whether they had health insurance. In addition, vaccination coverage generally increased as the number of physician contacts increased (e.g., influenza vaccination coverage among adults aged ≥19 years with health insurance was 24.0% for those without a physician contacts, 46.5% for those with 1-3 physician contacts, 58.0% for those with 4-9 physician contacts, and 59.4% for those with ≥10 physician contacts in the past 12 months. Among adults who had health insurance and ≥10 physician contacts within the past year, 21.0%–87.9% reported not having received a vaccine or vaccine series that were recommended either for all persons or for those with some specific indication. |
| Association of Respondent Age with Adult Vaccination Coverage | Box 4/ Table 6, Box 4/ Table 7, Box 4/ Table 8 | Influenza and pneumococcal vaccination coverage among adults ≥65 years was higher compared with coverage among adults 19–64 years; however, overall tetanus vaccination (Td or Tdap) and tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) coverage among adults ≥65 years was lower compared with coverage among adults <65 years. Hepatitis B vaccination coverage among adults with diabetes ≥60 years was lower compared with coverage among adults 19–59 years with diabetes. † Herpes zoster coverage among adults ≥65 years was higher compared with coverage among adults 60–64 years. |
| Adult Vaccination Coverage Adjusted for Selected Demographic and Access to Care Characteristics | Box 4/ Table 9 [1 sheet] Table 9 Ins-adjusted |
Adults without health insurance were less likely than those with health insurance to be vaccinated after adjusting for confounders for influenza (≥19 years); hepatitis A (≥19 years and travelers ≥19 years) ; hepatitis B (≥19 years and 19-49 years); and herpes zoster (≥60 years). |
| Adult Vaccination Coverage by Nativity, Years Living in the United States, and Citizenship | Box 4/ Table 10 [1 sheet] Table 10 Nativity |
Overall, vaccination coverage among U.S.-born respondents was higher than that of foreign-born respondents with few exceptions (influenza vaccination [adults all age groups], hepatitis A vaccination [adults ≥19 years], and hepatitis B vaccination [adults >19 years with diabetes; 19-59 years with diabetes; ≥60 years with diabetes]). Compared with U.S.-born adults, there were large gaps (>14 percentage points) in vaccination coverage among foreign-born adults for pneumococcal (>65 years), tetanus vaccination (all ages), Tdap vaccination (adults >19 years and 19-64 years), herpes zoster vaccination (>60 years and >65 years), and human papillomavirus (HPV) vaccination (females 19-26 years). Vaccination status among foreign-born adults varied by time living in the United States and citizenship. |
*Detailed information from these analyses is shown in Box 4_Disparities/ Tables 1-10 available at: AltText_Box4_Disparities [6 pages].
†In 2011, the Advisory Committee on Immunization Practices (ACIP) recommended hepatitis B vaccination for persons with diabetes 19–59 years and stated that persons with diabetes aged 60 years and older should be considered for vaccination.
Discussion
In 2017, adult vaccination coverage in the United States remained similar to that in 2016 for most vaccines. While modest coverage increases were noted for influenza and Tdap vaccination among adults overall, many adults remained unprotected against vaccine-preventable diseases. Influenza and pneumococcal vaccination coverage in adults with health conditions that increase the risk for complication from influenza or pneumococcal disease did not change between 2016 and 2017. Differences in coverage by race/ethnicity were observed for all vaccines in 2017, with white adults generally having higher coverage than non-white adults.
Millions of adults in the United States have conditions placing them at increased risk for complications of one or more vaccine-preventable infections56. Adults with certain chronic and immunocompromising health conditions are at substantially increased risk of invasive pneumococcal disease compared to adults without these conditions, with disease rates up to 20 times higher in some immunocompromised adults7. Similarly, adults with these conditions are significantly more likely to experience serious complications from influenza infection8. In this sample, only one-quarter of adults aged 19-64 years old at increased risk of invasive pneumococcal disease reported ever receiving a dose of pneumococcal vaccine. Although influenza vaccination coverage was higher in adults with high-risk conditions than those without, only 60% of adults at high risk of influenza complications were vaccinated in the 2016-2017 influenza season, leaving 40% of high-risk adults unprotected.
Studies indicate that a strong provider recommendation is closely associated with patient vaccination9. Wider adoption of the Standards for Adult Immunization1011 – assessing vaccination status at each adult patient visit, issuing strong recommendations for indicated vaccines, offering vaccines or referring patients to other providers for vaccination, and recording vaccinations received in an immunization information system – is likely to be helpful in improving vaccine coverage. Research suggests medical specialists are less likely than primary care clinicians to assess for, recommend, stock, or refer patients for needed vaccines12. Since patients with conditions placing them at increased risk of infection are likely to receive care from specialists, these encounters may represent missed opportunities for vaccination and could be addressed by consistent implementation of the Standards by these providers. Among the challenges clinicians face in assessing the need for vaccination is availability of a complete and accurate vaccination history along with access at the point of care to the most current immunization recommendations. Nationwide adoption of electronic health records, many of which have the capacity for patient-centered clinical decision support, also offer opportunities for improving adult vaccination rates2.
Composite performance measures, which combine multiple individual (“component”) quality measures, provide a useful way to examine overall health system performance in implementing standards of care as well as an incentive for implementation of these standards by providers3. The composite adult vaccination measure presented in this report has been adopted as a quality measure by the Indian Health Service and added to the Healthcare Effectiveness Data and Information Set (HEDIS) beginning in 2019313. The composite measure shows that despite variable coverage with individual recommended vaccines, few adults in any age group were fully vaccinated according to ACIP recommendations in 2017. Presentation of composite and component measures allows assessment of overall performance and targeted interventions to improve this performance; for example, Table 5 demonstrates that targeted efforts to improve Tdap vaccination coverage in adults aged ≥65 years could substantially increase the proportion of older adults who are fully vaccinated.
Large disparities in vaccination coverage by race/ethnicity have remained mostly unchanged over the last several years, with white adults having the highest coverage for most vaccines and age groups14. A variety of factors contribute to racial/ethnic differences in adult vaccination rates, including patient, provider, and system factors2. Standardized offering of vaccines reduces but does not eliminate these differences2. While programmatic initiatives designed to improve adult vaccine coverage overall may have a positive effect on these disparities15, their persistence in the face of years of such intervention suggests that novel and systematic approaches are required. More information on contributors to such disparities will be necessary to inform the design of meaningful interventions.
Despite increases in 2017 for certain vaccines or subpopulations, coverage with vaccines recommended for adults remains low. Achieving significant improvements in overall coverage while reducing racial/ethnic disparities will require action at multiple levels of the healthcare system. The new composite adult vaccination measure promises to facilitate the evaluation of interventions designed to reduce racial/ethnic disparities and increase the number of U.S. adults who are fully protected against vaccine-preventable diseases.
Limitations
The estimates in this report are subject to the following limitations. First, the NHIS sample excludes persons in the military and those residing in institutions, which might result in underestimation or overestimation of vaccination coverage levels. Second, all data rely on self-report and were not validated with medical records. However, adult self-reported vaccination status has been shown to be ≥70% sensitive in one or more studies for pneumococcal, tetanus toxoid-containing, herpes zoster, and hepatitis B vaccines and ≥70% specific in one or more studies for all except tetanus and hepatitis B vaccination161718. Third, adults might not be able to recall accurately vaccines received as infants or adolescents and as a result, coverage levels for hepatitis A, hepatitis B, HPV, and Tdap vaccination might be greatly underestimated. Additional studies are needed to determine accuracy of recall for vaccinations that adults may have received as children or adolescents. Fourth, the response rate was 53.0%. Nonresponse bias can result if respondents and non-respondents differ in their vaccination rates, and if survey weighting does not fully correct for this. Finally, Tdap estimates are subject to considerable uncertainty and potential for bias. Respondents who reported tetanus vaccination but were unable to say whether Td or Tdap was used (41.2%) were excluded from estimations of Tdap vaccination coverage.
- CDC. Immunization schedules for healthcare professionals: immunization for adults. Available at: www.cdc.gov/vaccines/schedules/hcp/imz/adult.html.
- Williams WW, Lu P-J, O’Halloran AO, et al. Surveillance of vaccination coverage among adult populations – United States, 2015. MMWR Surveill Summ 2017; 66 (SS-11):1-28.
- Shen AK, Williams WW, O’Halloran AC, et al. Promoting adult immunization using population-based data for a composite measure. Am J Prev Med 2018; 55(4):517-523.
- CDC. National Health Interview Survey public use data file. Available at: www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm.
- CDC. National Diabetes Statistics Report, 2017: Estimates of Diabetes and Its Burden in the United States. Available at www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf.
- CDC. National Chronic Kidney Disease Fact Sheet, 2017. Available at: www.cdc.gov/diabetes/pubs/pdf/kidney_factsheet.pdf.
- ACIP. Use of 13-Valent Pneumococcal Conjugate Vaccine and 23-Valent Pneumococcal Polysaccharide Vaccine for Adults with Immunocompromising Conditions: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep 2012; 61(40):816-819.
- ACIP Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices—United States, 2018–19 Influenza Season. MMWR Recomm Rep 2018; 67(No. RR-3):1–20.
- Bridges CB, Hurley LP, Williams WW, Ramakrishnan A, Dean AK, Groom AV. Meeting the Challenge of Immunizing Adults. Am J Prev Med 2015; 49(6S4):S455-S464.
- CDC. Standards for Adult Immunization Practice. Available at: www.cdc.gov/vaccines/hcp/adults/for-practice/standards/index.html.
- National Vaccine Advisory Committee. Recommendations from the National Vaccine Advisory Committee: standards for adult immunization practice. Public Health Rep 2014; 129:115–23.
- Lutz CS, Kim DK, Black CL, et al. Clinicians’ and Pharmacists’ Reported Implementation of Vaccination Practices for Adults. Am J Prev Med 2018; 55(3):308-318.
- NCQA. NCQA updates quality measures for HEDIS® 2019. Available at https://www.ncqa.org/news/ncqa-updates-quality-measures-for-hedis-2019/.
- Williams WW, Lu P-J, O’Halloran AO, et al. Surveillance of vaccination coverage among adult populations – United States, 2014. MMWR Surveill Summ 2016; 65 (No. SS-1):1-36.
- Schwartz KL, Neale AV, Northrup J, et al. Racial similarities in response to standardized offer of influenza vaccination: A MetroNet study. J Gen Intern Med 2006; 21(4):346-351.
- Rolnick SJ, Parker ED, Nordin JD, et al. Self-report compared to electronic medical record across eight adult vaccines: do results vary by demographic factors? Vaccine 2013;31(37):3928-3935.
- Donald RM, Baken L, Nelson A, Nichol KL. Validation of self-report of influenza and pneumococcal vaccination status in elderly outpatients. Am J Prev Med 1999;16:173-177.
- Zimmerman RK, Raymund M, Janosky JE, et al. Sensitivity and specificity of patient self-report of influenza and pneumococcal polysaccharide vaccinations among elderly outpatients in diverse patient care strata. Vaccine 2003;21:1486-1491.
